Summary Card
Definition
A congenital deformity characterized by constricted, elevated, herniated, and hypoplastic features, while maintaining normal function.
Clinical Features
Features vary widely, commonly including asymmetry, hypoplasia, constricted base, IMF elevation, herniated nipple, ptosis, and skin envelope insufficiency.
Classification
Von Heimburg's 1996 system is crucial for assessing the condition, emphasizing the identification of specific affected areas to inform surgical strategies.
Surgery
Aims to release constrictions, restore volume, reposition the inframammary fold, and achieve symmetry, involving techniques like periareolar incisions, radial scoring, and dual-plane pocket creation, and may require single or two-stage procedures depending on severity.
Primary Author:
Dr Kurt Lee Chircop, Plastic Surgery Trainee, Malta
Definition of Tuberous Breasts
Tuberous breast is a congenital deformity characterized by a constricted, elevated, herniated, and hypoplastic appearance, with normal function retained.
A "tuberous breast" is a congenital breast deformity that results in a constricted, elevated, herniated and hypoplastic breast (Rees, 1976). The breast maintains normal function and physiology.
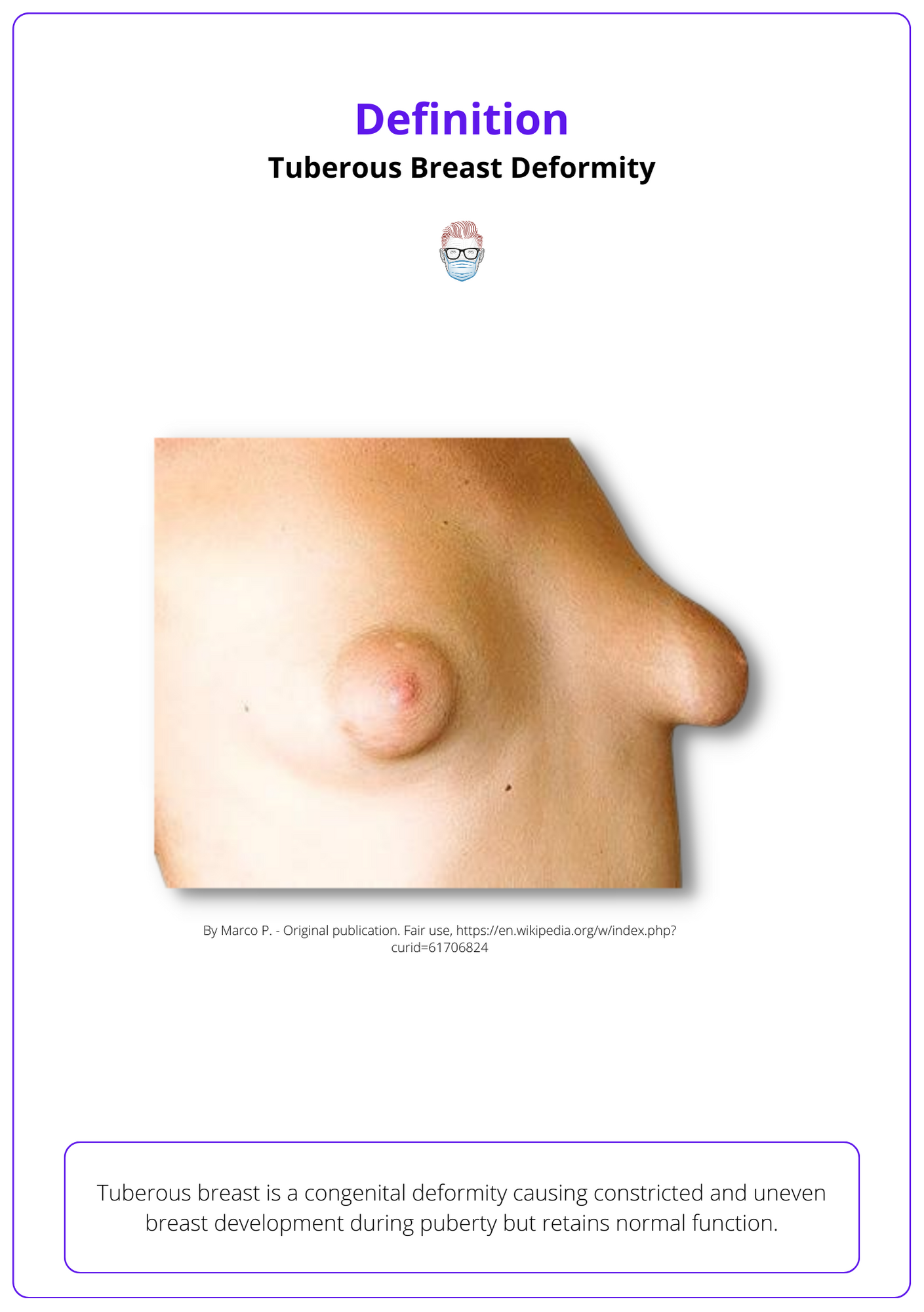
True incidence is unknown in view of significant under-reporting, especially with the minor forms of the spectrum of deformity. Typically found in patients presenting for breast augmentation or mastopexy with incidence of 30-50% (Klinger, 2016)
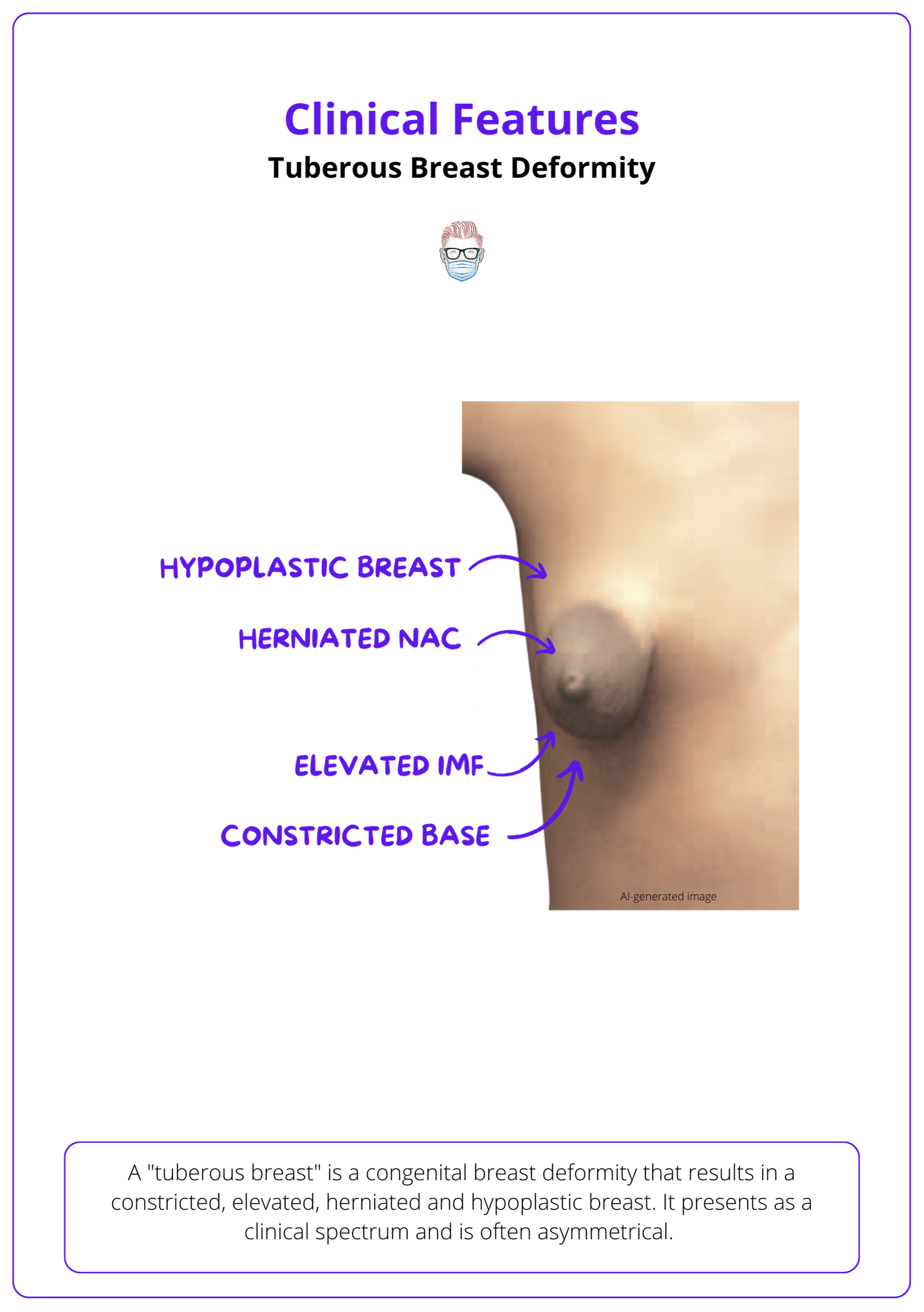
Clinical Features of Tuberous Breasts
Tuberous breast deformity features asymmetry, hypoplasia, constriction, and ptosis, making accurate diagnosis crucial for effective aesthetic correction beyond just volume increase.
Tuberous breast deformities present on a clinical spectrum. The condition can be unilateral or bilateral and is very commonly asymmetric in nature.
The key clinical findings include the following:
- Volume: parenchymal hypoplasia and asymmetry.
- Base constricted: deficient width (horizontal) and height (vertical)
- IMF: medial and or lateral elevation; complete absence.
- Nipple: herniated and widened
- Ptosis: mild to severe, often defies standard classification.
- Skin envelope: insufficiency, typically inferior pole.
Below image identifies the clinical features of Tuberous Breast Deformity.
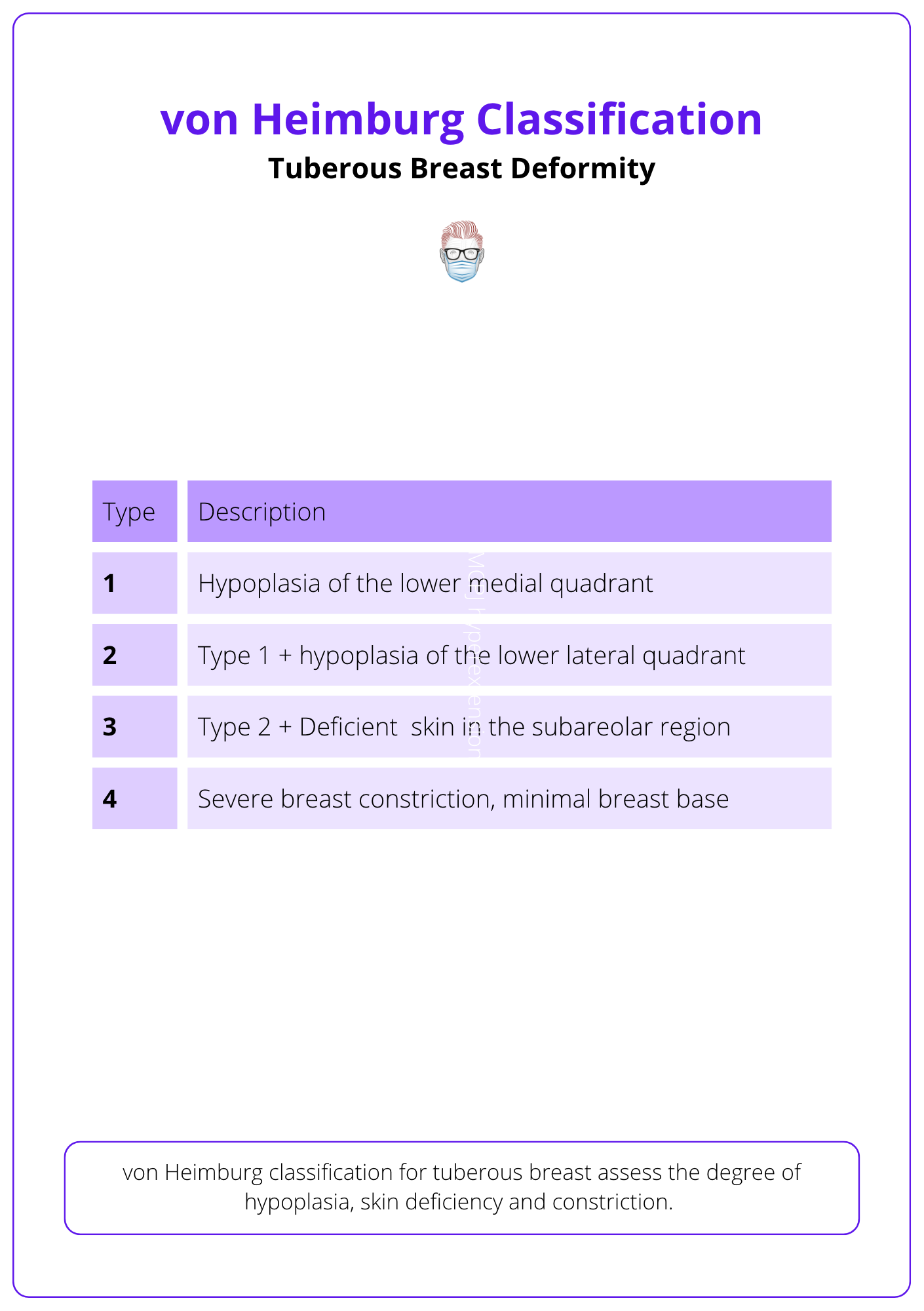
Classification of Tuberous Breasts
Von Heimburg's 1996 classification is key for accurately assessing and predicting outcomes of tuberous breast deformity by detailing specific affected areas.
Precise nomenclature and classification are crucial for preoperative assessment of tuberous breast deformity, enabling the identification of specific characteristics and their severity to ensure more predictable outcomes.
Among the various classification systems Von Heimburg's 1996 framework has been popularised. It categorises the deformity based on the affected areas (von Heimburg, 1996)
Surgery for Tuberous Breasts
Tuberous breast correction surgery involves periareolar incision for precise adjustments, radial scoring to release constrictions, and dual-plane pocket creation for optimal shape, with procedures varying from single to two-stage based on individual needs for achieving desired breast volume and symmetry.
Goals of Surgery
For patients dissatisfied with their breast shape or size due to tuberous deformity, surgical correction aims to:
- Release constrictions.
- Restore breast volume.
- Reposition the inframammary fold.
- Achieve symmetry.
Typically, a single-stage procedure suffices, leveraging the distensibility of soft tissues. However, for severe cases or when larger volumes are desired and tissues lack pliability, two-stage procedures with expanders may be necessary.
Check out these below video for more insights on the surgical procedure for Tuberous Breasts.
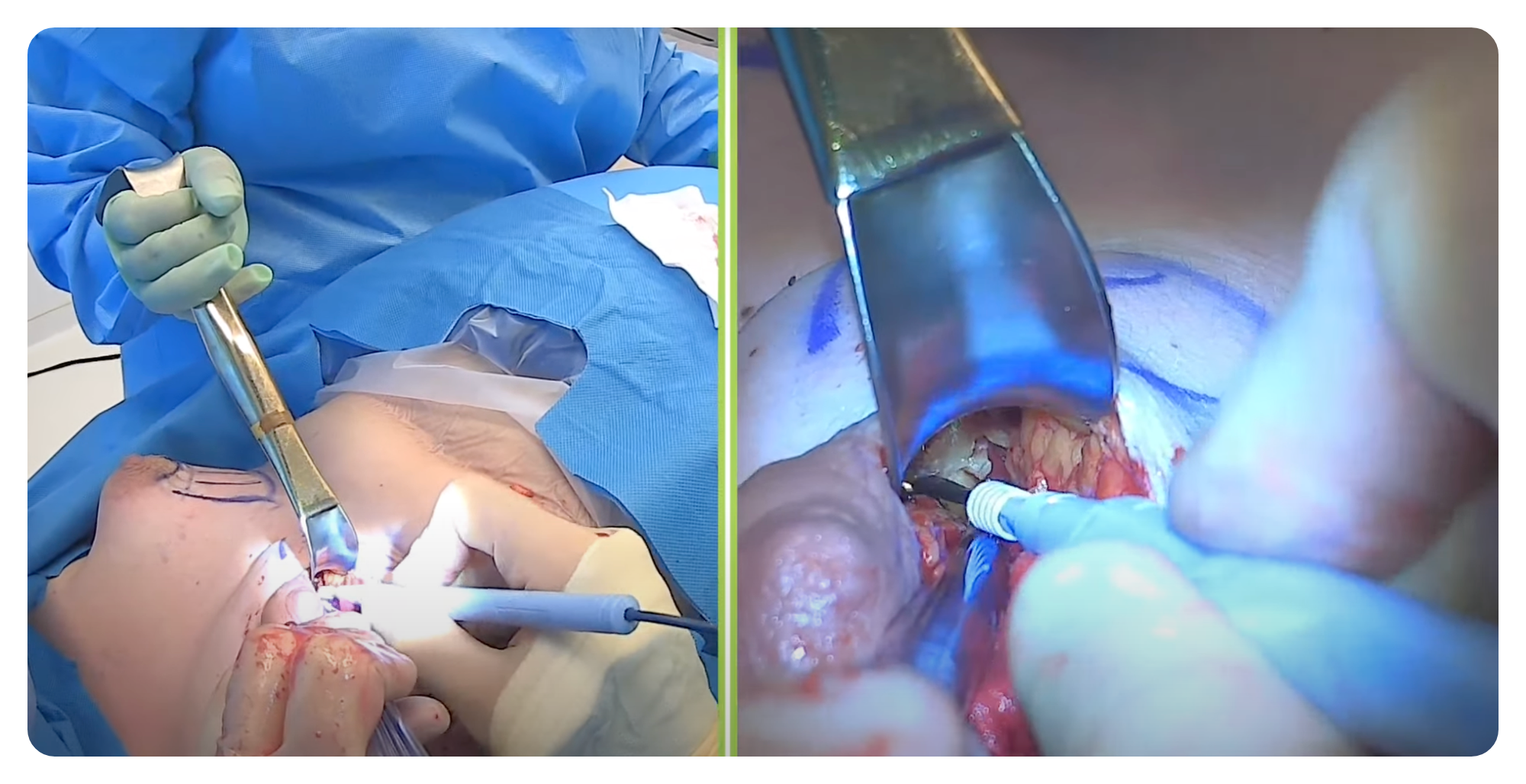
Overview of Surgical Technique
This guide outlines common steps in tuberous breast correction surgery, noting that techniques may vary among surgeons.
- Periareolar Skin Incision: Allows areolar reduction, access to the subglandular plane, and radial release of constriction rings.
- Dissection: Proceeds down to the subglandular prefascial plane, extending inferiorly to the new inframammary fold (IMF) position.
- Radial Scoring: Involves radial incisions into the glandular tissue perpendicular to the subglandular layer, particularly at the lower pole to release constrictions and facilitate expansion.
- IMF Positioning: Through transglandular dissection to the prepectoral fascial plane, defining the new lower limit of the breast.
- Pocket Creation: Establishes a dual-plane pocket via a horizontal incision in the lower part of the pectoralis major muscle, combined with retropectoral dissection, resulting in a Dual-Plane Type 3 pocket.
- Volume Replacement: Selection between implants or expanders, round versus anatomical shapes. Utilizes a sizer with tailor tacking before final insertion.
- NAC (Nipple-Areola Complex) Herniation/Ptosis Correction: Employs circumareolar and/or vertical mastopexy techniques, either immediate or delayed. This includes concentric de-epithelialization for areolar size reduction and circumareolar mastopexy using round-block suturing.
Specific Aspects to Surgery
Skin Incision
A periareolar incision is crucial for precise breast reshaping, combining flexibility and predictability. Advantages include:
- Allowing precise inframammary fold adjustment.
- Providing direct access to correct glandular constrictions.
- Effective in treating herniation, enlarged NAC, and ptosis.
Radial Scoring
Radial scoring involves transglandular dissection towards the prepectoral fascia, extending to the new lower breast boundary. This method targets the constricting fascial bands, employing perpendicular (vertical/radial) cuts from the subglandular layer, aiming to:
- Expand the breast's lower pole.
- Visually eliminate the memory of any preexisting inframammary fold.
In cases of severe constriction, subdermal scoring may be employed for enhanced results.
Pocket Creation
The dual-plane technique, combining the benefits of both submuscular and subglandular placements, is favored for tuberous breast corrections. It facilitates lower pole expansion and shaping while maintaining minimal fill in the upper pole, allowing the muscle to move up, away from the adjusted inframammary fold (IMF). This approach enhances the natural contour, improves soft-tissue coverage, stabilizes breast position, and reduces the risk of capsular contracture.
Conversely, subglandular placement directly shapes and expands the breast but can lead to:
- Higher capsular contracture rates.
- Visible implant edges and rippling.
- Risk of implant malposition.
- Unnatural appearance, particularly due to the scoring and thinning required in tuberous breast correction.
Single-stage vs Two-stage
In tuberous breast correction, choosing between single-stage and two-stage procedures depends on individual patient factors and desired outcomes:
Single-stage correction is suitable for patients with distensible lower pole skin and soft tissues who have conservative size expectations. This approach allows for immediate correction and repositioning of the breast tissue and inframammary fold in a single procedure.
Two-stage correction, involving initial tissue expander placement followed by implant insertion, is recommended for:
- Patients desiring a fuller outcome with moderate to severe breast hypoplasia.
- Situations where overcoming the memory of the preexisting inframammary fold is challenging.
- Cases with severe constriction and superior malposition of the inframammary fold, allowing for a secondary "fine-tuning" procedure to enhance breast symmetry and achieve optimal aesthetic results.
Conclusion
1. Nature of Tuberous Breast Deformity: Acquired knowledge of tuberous breasts, a congenital condition characterized by a variety of physical manifestations including asymmetry, constricted base, and herniated nipple, while maintaining normal breast function.
2. Clinical Features and Diagnosis: Enhanced the ability to recognize the clinical features of tuberous breasts, crucial for accurate diagnosis and effective aesthetic correction, acknowledging the condition's spectrum from asymmetry and hypoplasia to ptosis and skin envelope insufficiency.
3. Classification of Tuberous Breast Deformity: Learned about Von Heimburg's 1996 classification system, an essential tool for assessing tuberous breast deformity, facilitating the identification of specific areas affected to inform tailored surgical strategies.
4. Surgical Interventions: Gained insights into the surgical goals and techniques for correcting tuberous breasts, including the importance of releasing constrictions, restoring volume, repositioning the inframammary fold, and achieving symmetry, with the choice between single or two-stage procedures tailored to the severity of the condition and patient desires.
Further Reading
- Klinger M, Caviggioli F, Giannasi S, Bandi V, Banzatti B, Veronesi A, Barbera F, Maione L, Catania B, Vinci V, Lisa A, Cornegliani G, Giaccone M, Siliprandi M, Klinger F. The Prevalence of Tuberous/Constricted Breast Deformity in Population and in Breast Augmentation and Reduction Mammaplasty Patients. Aesthetic Plast Surg. 2016 Aug;40(4):492-6. doi: 10.1007/s00266-016-0650-9. Epub 2016 Jun 6. PMID: 27271839.
- Pacifico MD, Kang NV. The tuberous breast revisited. J Plast Reconstr Aesthet Surg. 2007;60(5):455-64. doi: 10.1016/j.bjps.2007.01.002. Epub 2007 Feb 21. PMID: 17399653.
- Rees TD, Aston SJ. The tuberous breast. Clin Plast Surg. 1976 Apr;3(2):339-47. PMID: 1261187.
- von Heimburg D, Exner K, Kruft S, Lemperle G. The tuberous breast deformity: classification and treatment. Br J Plast Surg. 1996 Sep;49(6):339-45. doi: 10.1016/s0007-1226(96)90000-4. PMID: 8881778.


