Summary Card
Anatomy of Lip Reconstruction
The lip is composed of skin, muscle, and mucosa. Its blood supply is the labial arteries.
Principles of Lip Reconstruction
Restore the layers of the lip. Key landmarks to preserve include the philtrum, modiolus, cupid's bow, and vermillion.
Lip Reconstruction Options
The lip can be reconstructed by primary closure, local flap, or free flap. This depends on the patient and the lip defect (size and location).
Primary Lip Closure in Lip Reconstruction
Defects <1/3 of the lip and appropriate soft tissue laxity.
Abbe Lip Switch Flap
Defects <1/3 of the lip and an intact commissure.
Abbe-Estlander Flap
Defects <1/3 of the lip and an involved commissure.
Karapandzic Flap
Central defects <2/3 of the upper and lower lip.
Bernard-Burow Cheiloplasty
Central defect >2/3 of the lower lip, causes incompetence & microstomia.
Free Flap Reconstruction
Radial forearm flap to reconstruct the entire lip. There is no motor innervation, and cosmesis can be poor.
Anatomy of Lip Reconstruction
The lip is composed of skin, muscle, and mucosa. It is supplied by the labial arteries. Key landmarks include modiolus, cupid's bow, vermillion, and philtrum.
Lip reconstruction recreates the skin, muscle, and mucosa elements of the lip to maintain oral competence, speech, and cosmesis.
The neurovascular anatomy of the lip is detailed below.
- Motor: buccal and mandibular branches of the facial nerve.
- Sensory: infraorbital (upper), mental (lower) branches of trigeminal nerve.
- Blood supply: superior and inferior labial branches of the facial artery.
The landmarks of the lip are illustrated below.

Principles of Lip Reconstruction
Lip reconstruction should restore the layers of the lip. There are key anatomical landmarks that should also be preserved.
"Restoration is designed from within.... the mucosal lining should be considered first, then the supporting structures, and then finally the skin covering". This was outlined in Sir Harold Gilles's seminal publication, as illustrated below.
Lip Reconstruction Options
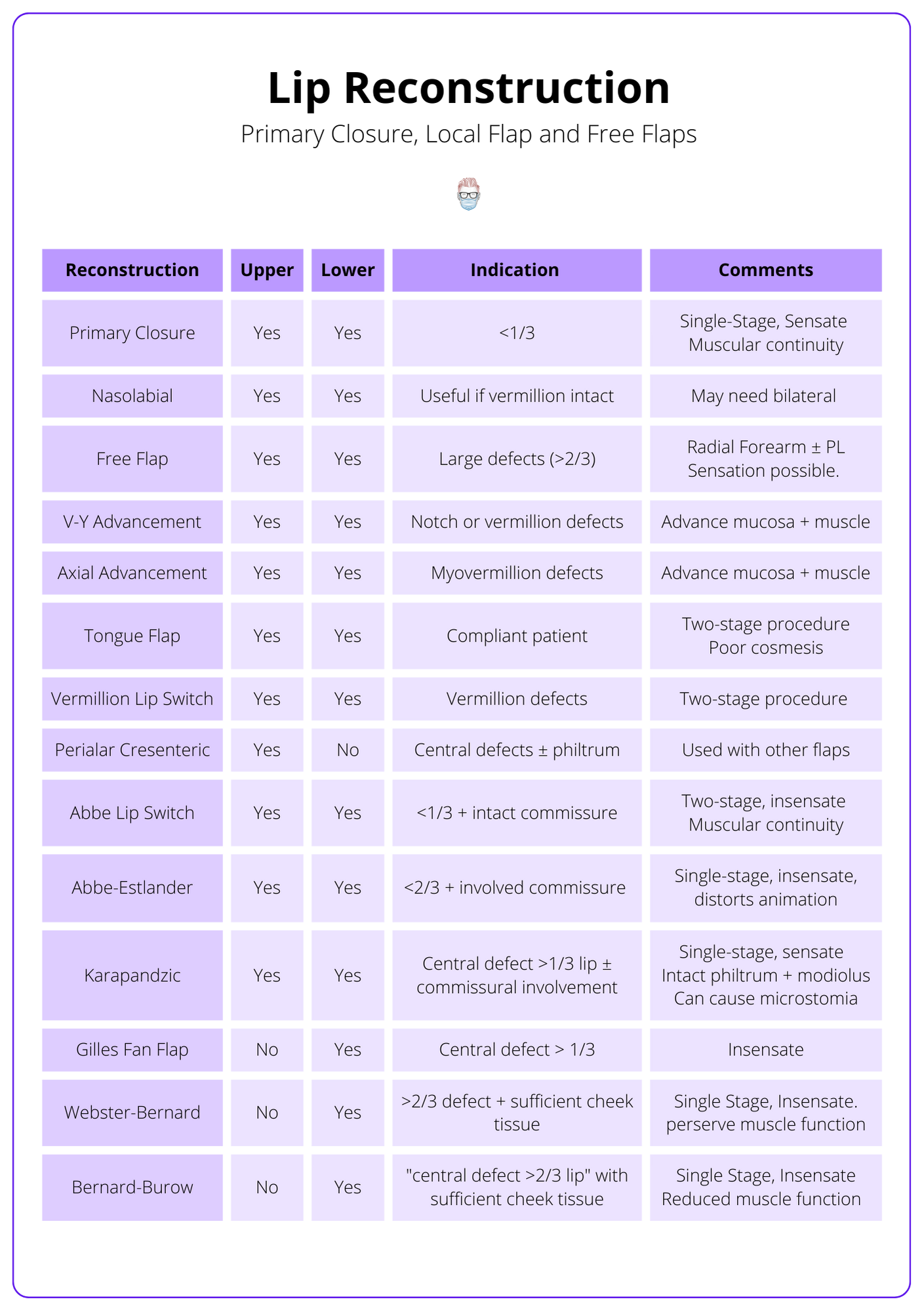
Lip reconstruction is guided by the location, size, and depth of the defect. Reconstructive options include primary closure, local flap, or free flap. Landmarks, competence, and function should be preserved when possible.
Lip reconstruction should aim to restore "like with like". The reconstruction is dependent on the following factors:
- Location: upper lip vs lower lip, central vs lateral vs commissural.
- Size and depth: <1/3 vs <2/3, skin vs mucosal vs muscle, vermillion.
- Goals: function vs cosmesis vs maintaining oral aperture (important for dentures).
The lip reconstructive options are illustrated in the table below.
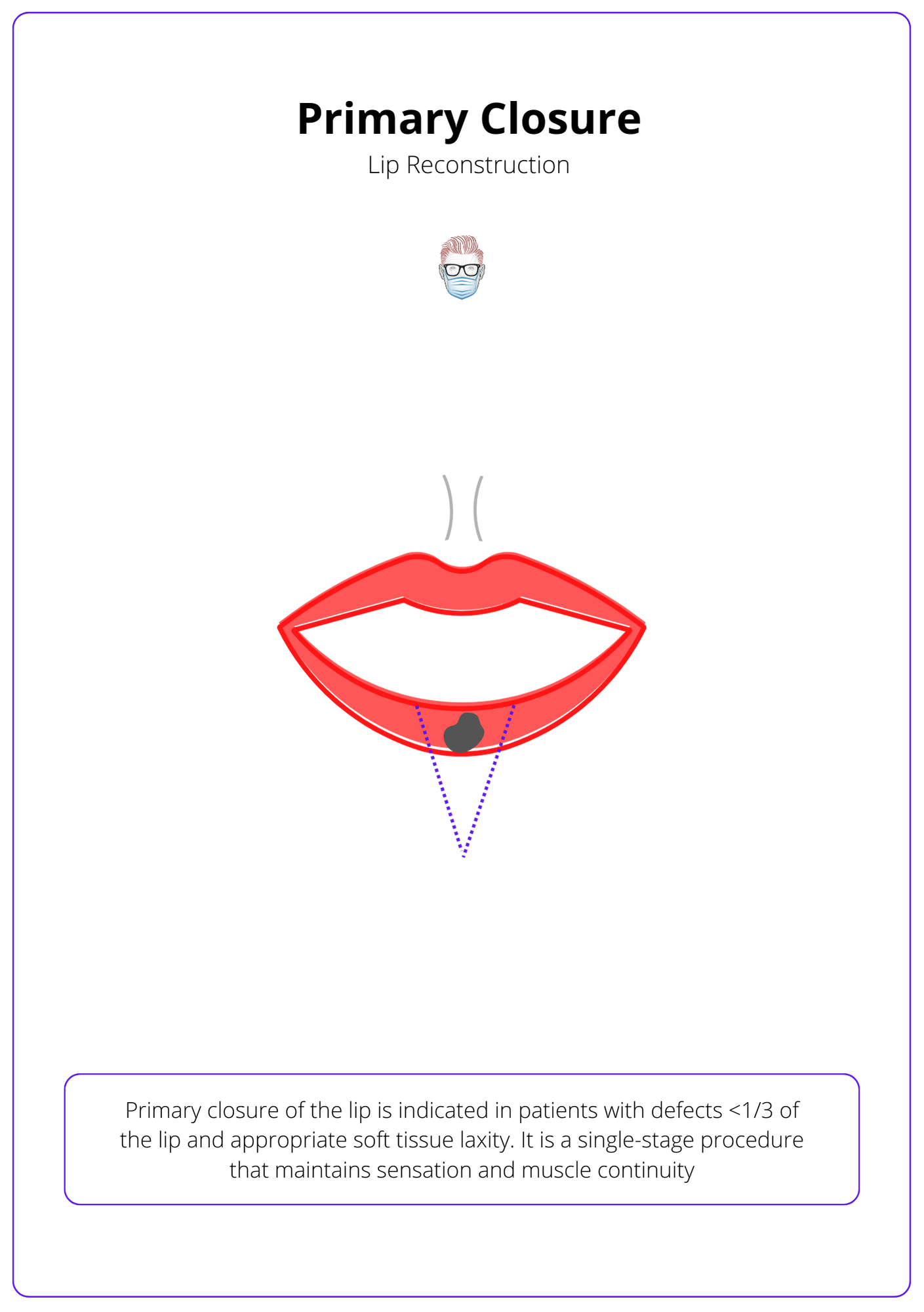
Primary Lip Closure in Lip Reconstruction
Primary lip closure is used for defects less than one-third of the lip, following wedge excision of lesions. It maintains muscle continuity and innervation in a single stage.
This is indicated in patients with defects <1/3 of the lip and appropriate soft tissue laxity. It is commonly used after wedge excision of lip lesions, such as squamous cell carcinoma.
- Indications: defect <1/3 of the lip and appropriate soft tissue laxity.
- Benefit: single-stage, innervated, muscle continuity.
- Limitations: small defects, can remove cupid's bow/philtrum.
- Design: Realign all layers of the lip (skin, muscle, and mucosa).
Primary lip closure is better illustrated in the image below.
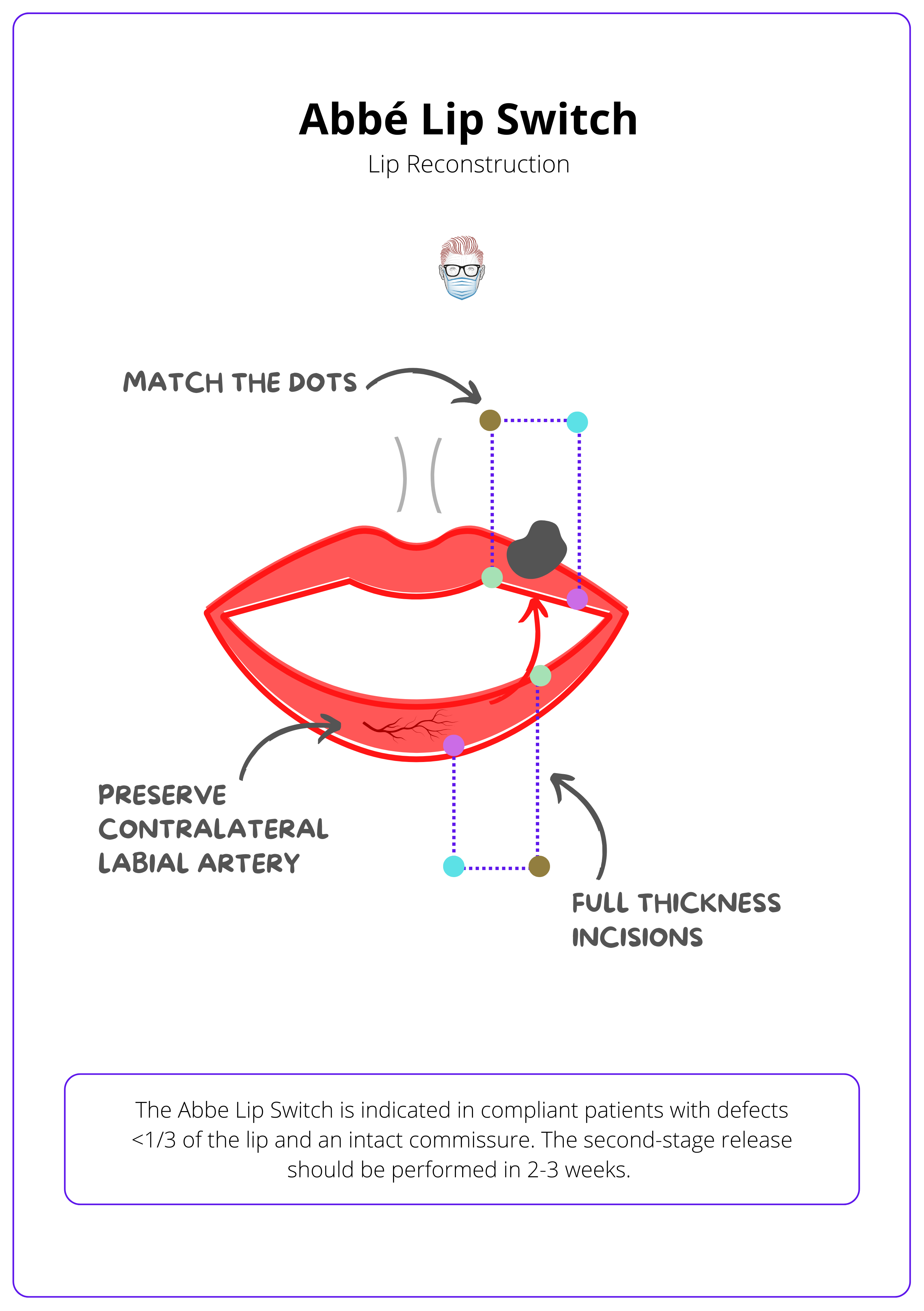
Abbe Lip Switch Flap
This is indicated in compliant patients with defects <1/3 of the lip and an intact commissure. The second-stage release should be performed in 2-3 weeks.
Abbe Lip Switch Flap is a refined surgical technique designed for patients with specific lip defects. This is ideal for defects that are less than one-third of the lip's length and when the commissure remains intact.
- Indications: defect <1/3 of the lip + intact commissure + compliant patient.
- Benefit: muscle continuity, preserves landmarks (cupid's bow, philtrum, modiolus).
- Limitations: two-stage, insensate.
- Design: full thickness, half the defect width, based on ipsilateral labial artery.
- Tip: protect the labial artery with a cuff of muscle and ensure adequate mouth opening during the 2-week period between the first and second stages.
The anatomy of the Abbe Lip Switch Flap is illustrated below.
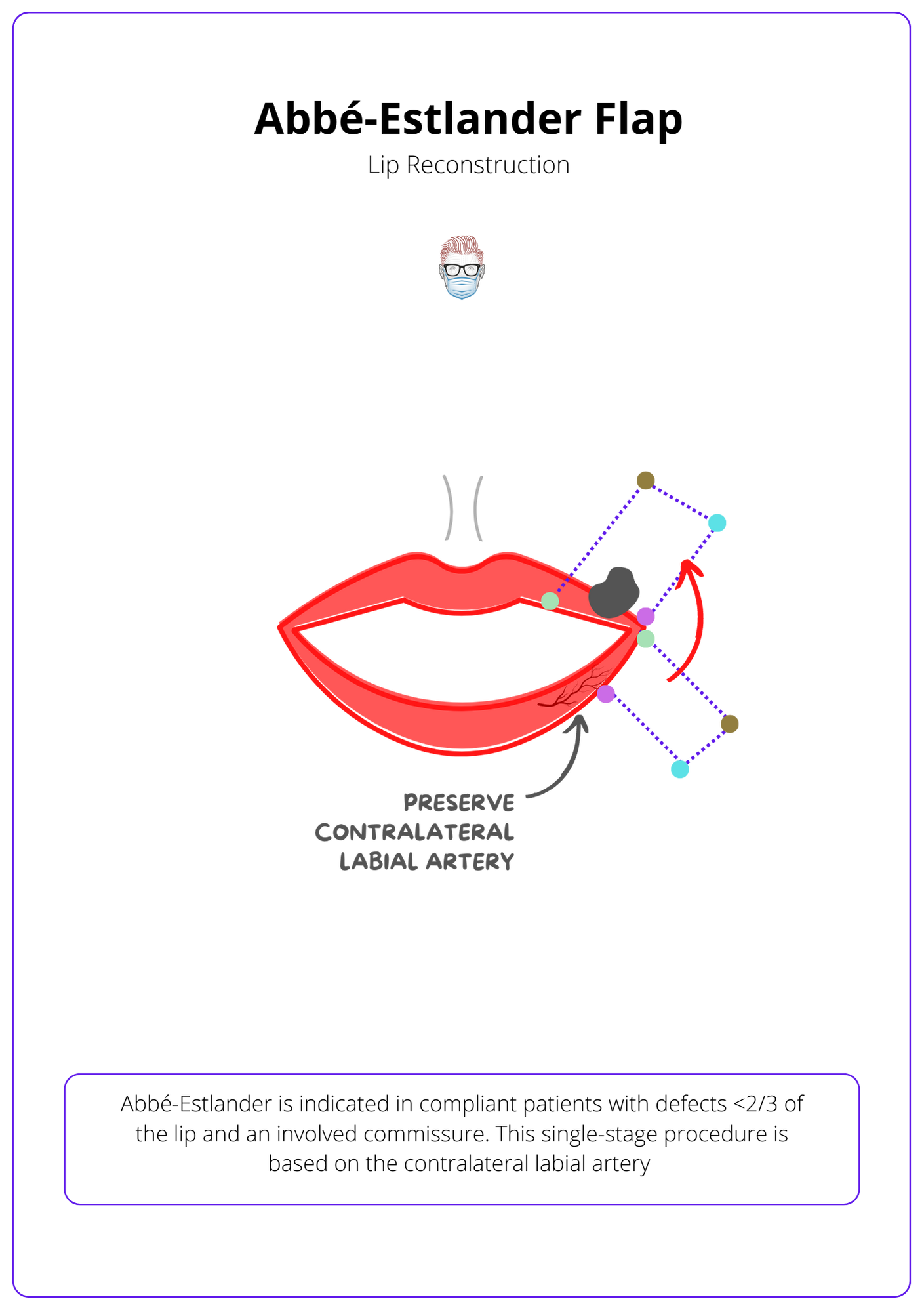
Abbe-Estlander Flap
This is indicated in compliant patients with defects <1/3 of the lip and an involved commissure. The second-stage release should be performed in 2-3 weeks.
This surgical approach is ideal for patients with lip defects under two-thirds and involving the commissure, allowing for a potential single-stage process.
- Indications: defect <2/3 of upper and lower lip + commissure affected.
- Benefit: single-stage is possible.
- Limitations: insensate, can distort oral animation as modiolus altered.
- Design: full thickness, third-half defect width, contralateral labial artery.
- Tip: protect the labial artery with a cuff of muscle; it may require secondary commissuroplasty.
The image below illustrates the mechanism of the Abbe-Estlander Flap.
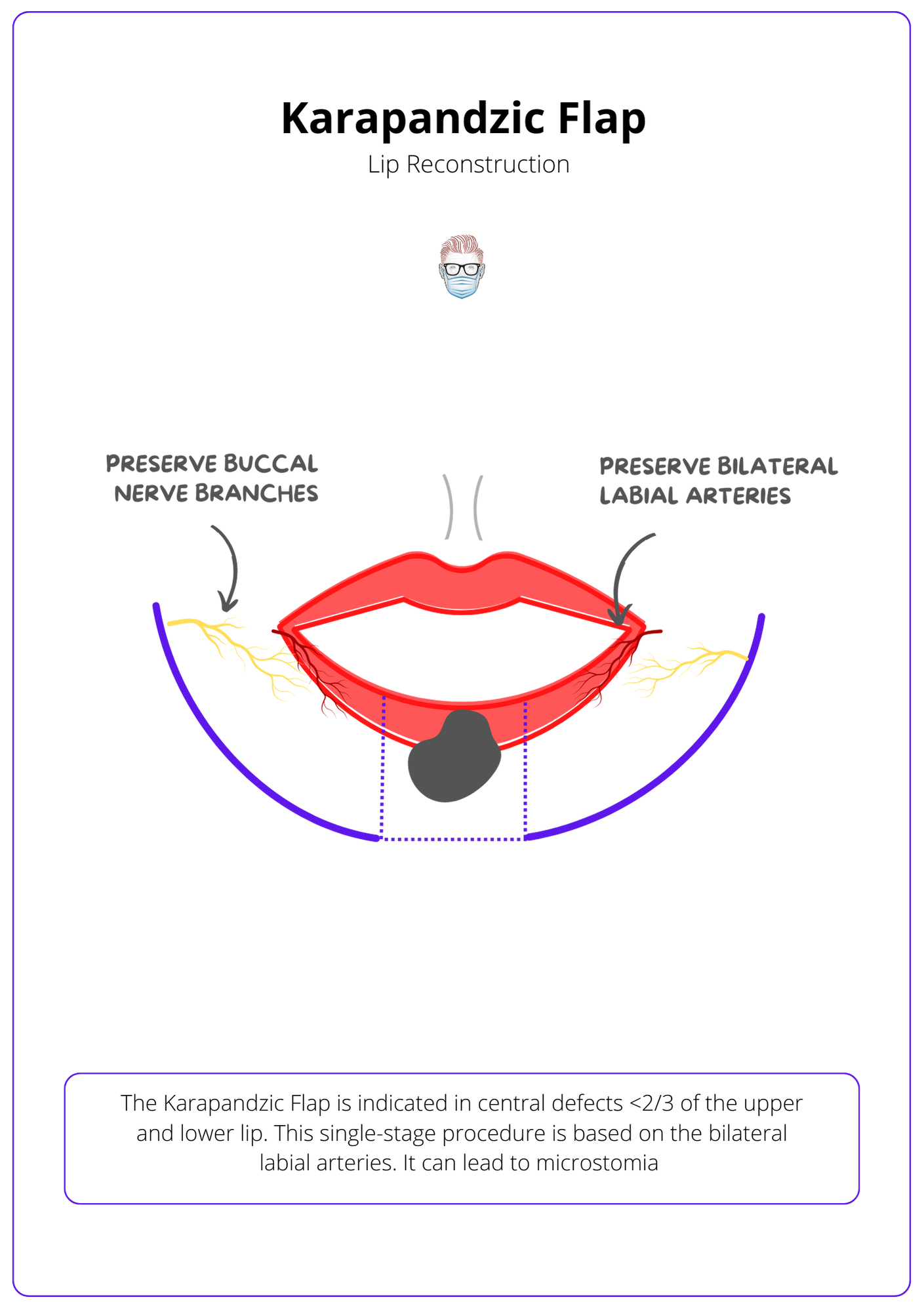
Karapandzic Flap
This is indicated in central defects <2/3 of the upper and lower lip. This single-stage procedure is based on the bilateral labial arteries. It can lead to microstomia.
The karapandzic flap is an orbicularis oris myocutaneous flap with an axial blood supply.
- Indications: central defect <2/3 of upper and lower lip.
- Benefit: single-stage, sensate, preserves oral competence and landmarks (philtrum and modioulus).
- Limitations: can lead to microstomia.
- Design: rotational, circumoral flaps based on the bilateral labial arteries.
- Tip: preserve the vascular pedicles and buccal branches by performing intramuscular dissection.
Karapandzic Flap lip reconstruction is illustrated below.
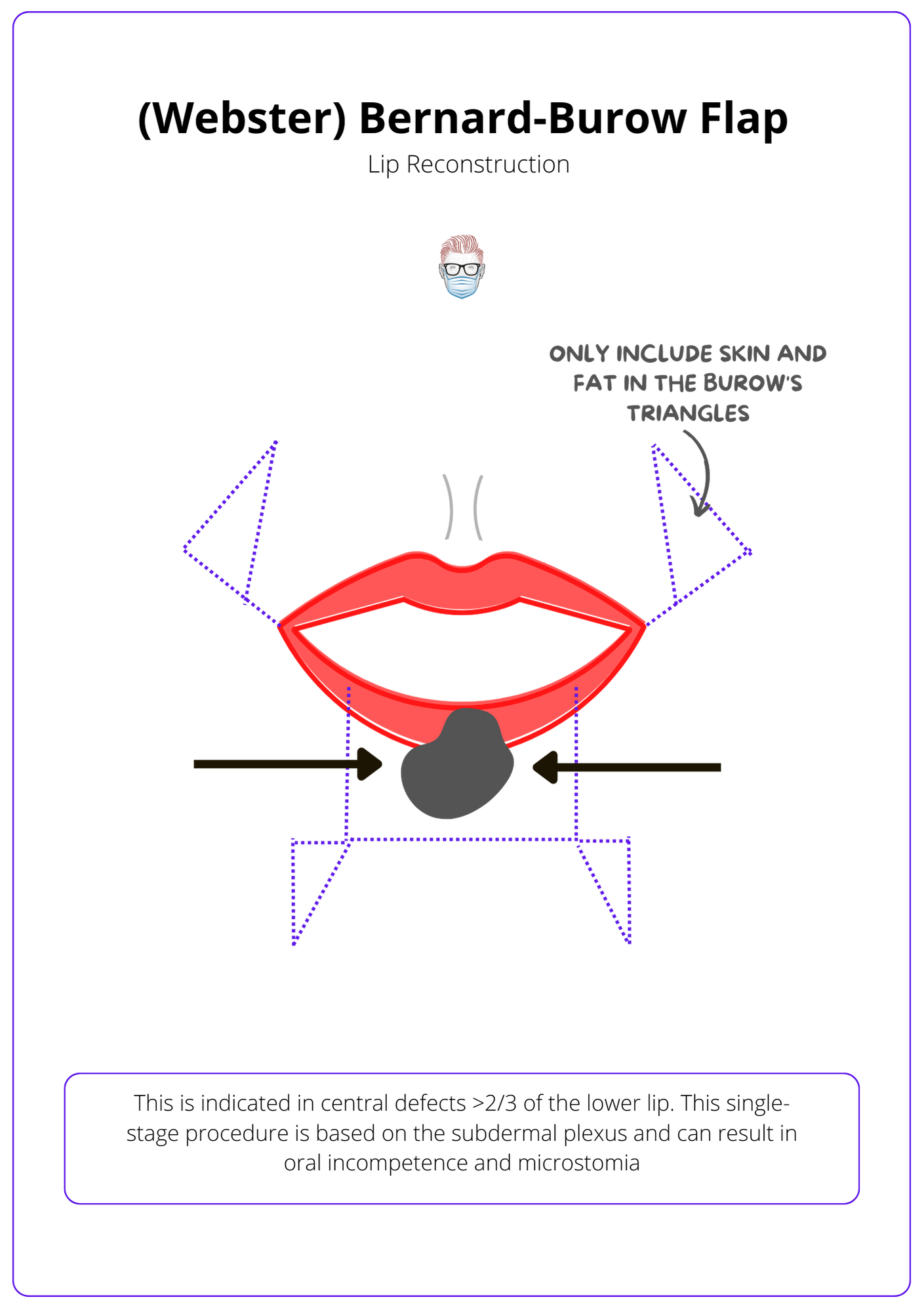
Bernard-Burow Cheiloplasty
This is indicated in central defects >2/3 of the lower lip. This single-stage procedure is based on the subdermal plexus and can result in oral incompetence and microstomia.
This procedure, efficient in its single-stage approach, utilizes the subdermal plexus for the medial advancement of the cheek with innovative Burow's triangles.
- Indications: central defect >2/3 of the lower lip.
- Benefit: single-stage.
- Limitations: insensate, can lead to oral incompetence and microstomia.
- Design: medial advancement of the cheek with Burow's triangles.
- Tip: based on facial subunits and the dermal plexus.
The Bernard-Burow Flap is illustrated in the image below.
Free Flap Reconstruction
The radial forearm flap can be considered for reconstructing the entire lip in patients with irradiated tissue (post-tumour resection). There is no motor innervation, and cosmesis can be poor.
The Radial Forearm Flap is a choice for reconstructing the entire lip, particularly in patients with tissue damage from radiation post-tumor resection.
- Indications: total or near total loss of the lip.
- Benefit: good soft tissue coverage with potential for sensation with lateral antebrachial cutaneous nerve.
- Limitations: no motor innervation, poor cosmesis (colour and lip landmarks).
- Design: radial forearm and palmaris longus.
- Tip: consider in patients after tumour resection and radiotherapy to local tissues.
There are currently published case reports on the role of an innervated gracilis muscle in providing a functional lower lip. The radial forearm and palmaris longus is illustrated below.
Conclusion
1. Lip Anatomy and Landmarks: You've gained a detailed understanding of the functional and aesthetic components that make up the lip, including the skin, muscle, mucosa, and critical vascular supply.
2. Lip Reconstruction Principles: You've learned about the principles of lip reconstruction which emphasize restoring the lip's three layers while preserving key anatomical landmarks like the philtrum, modiolus, cupid's bow, and vermillion for both functional and cosmetic purposes.
3. Reconstruction Techniques Overview: You've gained knowledge on various surgical techniques for lip reconstruction, tailored to the extent and location of the defect.
4. Specific Surgical Options: You've reviewed surgical options including the Abbe Flap, Karapandzic Flap, Bernard-Burow Cheiloplasty, and others, understanding their indications, benefits, and limitations.
5. Decision Making in Lip Reconstruction: Finally, you've learned how to apply these concepts in clinical practice, considering factors such as the size of the defect, the involvement of key structures, patient-specific factors, and desired outcomes to select the most appropriate reconstructive strategy.


