Summary Card
Classification of Mandibular Defects
Jewer-Boyd classification is used to describe hemi-mandibular, central, and lateral defects. It guides the therapeutic algorithm.
Pathophysiology of Mandibular Invasion
Directly in lymphatics or via nerves. Periosteum and teeth provide relative resistance to invasion.
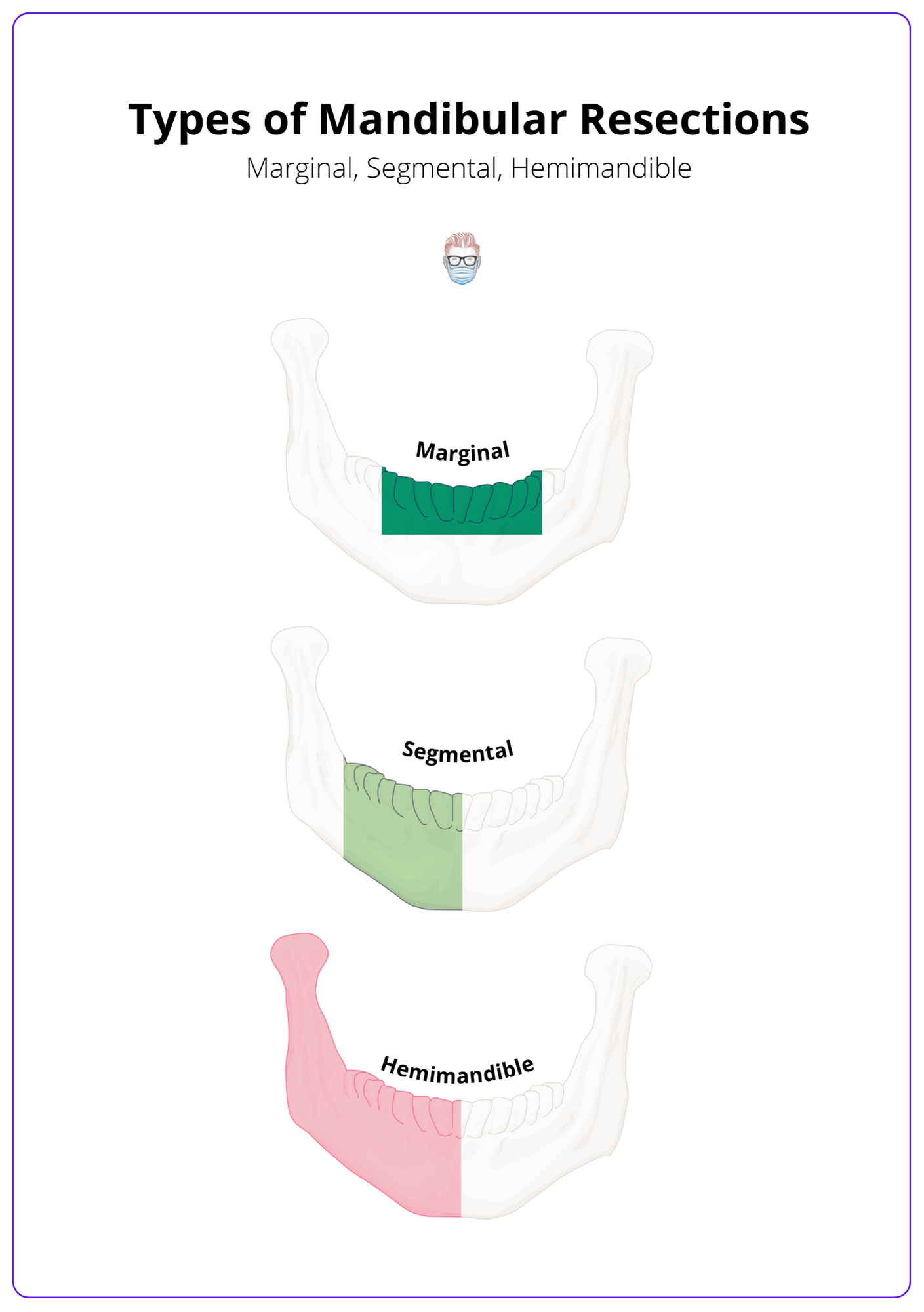
Types of Mandibular Resections
3 types based on their width and length of resection: marginal (rim), segmental, and hemimandile.
Types of Mandibular Reconstruction
No reconstruction, plates, non-vascularised bone grafts, and vascularized bone flaps.
Classification of Mandibular Defects
The Jewer-Boyd classification is most commonly used to describe hemi-mandibular, central and lateral defects. It guides the therapeutic algorithm.
The classification of mandibular defects provides a standardised communication tool and guides the therapeutic algorithm for the reconstruction. There are several classification systems, but Jewer-Boyd is the most widely accepted in clinical practice (Boyd et al., 1993).
Jewer-Boyd Mandibular Classification (H-C-L)
In 1989, Jewer and Boyd described the HCL classification for hemimandibular (H), central (C), and lateral (L) defects of the mandible. Boyd modified this classification to include mucous (M) and/or skin (S) involvement.
- Hemimandibular: lateral and horizontal segments including the condyle of any length and not significantly crossing the midline.
- Central: segment between the incisive foramen (2 canines and 4 incisors).
- Lateral: segment not including the condyles.
This HCL mandible classification is seen in the image below.
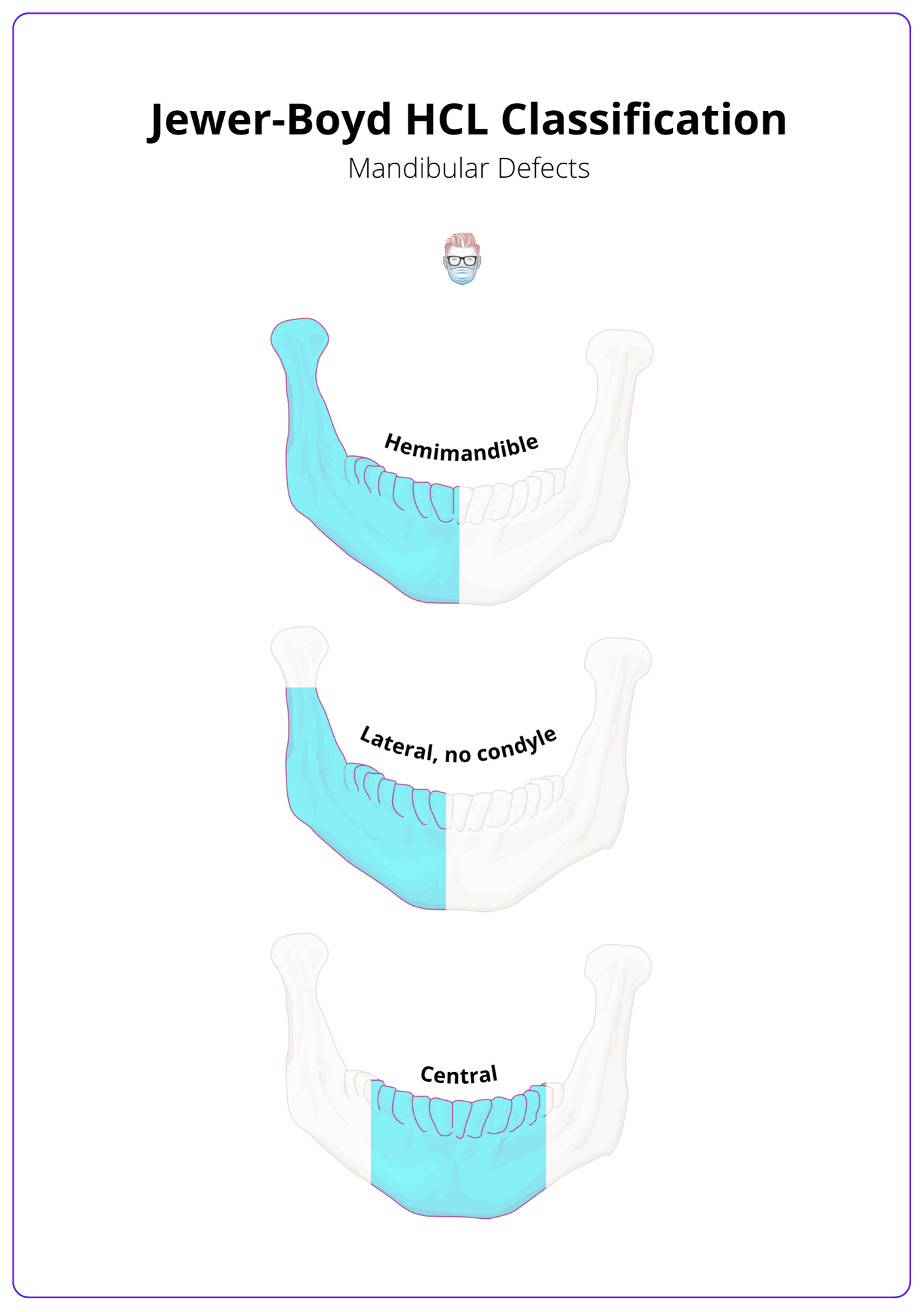
The length of the defect is not included in this mandibular classification. In reality, many mandibular defects are a combination — for example, LCL.
Other Mandibular Classifications
- CRBS by Urken (1991) assessed the bone (condyle, ramus, body, and symphysis), soft tissue (lip, buccal, soft palate, floor of the mouth, tongue, and skin), and nerve (inferior alveolar, lingual, hypoglossal nerve, and facial nerve).
- Schultz (2015) assesses a defect's dentate nature of alveolus and ramus, unilateral or bilateral, laterality of the donor's vessels, and condylar involvement.
- Brown (2016) defines four classes of segmental mandibulectomy: lateral, hemimandibulectomy, anterior, and extensive ± condylectomy.
There is no "perfect" mandibular classification system, and its complexities can make it challenging to apply in routine practice.
Pathophysiology of Mandibular Invasion
Invasion of the mandible can occur directly, in lymphatics or via nerves. Periosteum and teeth to provide relatively resistant to invasion.
Mechanisms
Generally speaking, mone invasion occurs via:
- Soft tissues: infiltrative spread
- Lymphatic: embolic spread
- Nerves: permeative spread
- Occlusal surfaces: direct after tooth extraction
Role of Teeth
The mechanism of tumour invasion is different for dentate and edentulous mandibles.
- Dentate mandible: invasion occurs via tooth sockets.
- Edentulous mandible: invasion via occlusal surface and alveolar bone resorption provide a shorter route.
Types of Mandibular Resections
3 types of mandibular resections based on their width and length of resection: marginal (rim), segmental, and hemimandible.
Mandibular resections can be classified into 3 different types of mandibulectomies based on their width and length of resection: marginal (rim), segmental, and hemi-mandible. Their relative indications are determined by physical examination and radiographic imaging after discussion at a multidisciplinary meeting.
The types of mandibular resections can be seen in the image below.
Factors to Consider
The management options for mandibular resection should take into consideration the following variables:
- Tumour: location in relation to the mandible.
- Mandible: dentate or edentulous, atrophy, radiotherapy.
- Patient: comorbidities and outcome expectations.
Marginal (Rim)
A marginal rim resection of the alveolus ± lingual plate with body and inferior alveolar nerve preservation. It can be considered in the following patients after discussion at a multidisciplinary meeting.
- Mandibular adjacent.
- Mandibular periosteum invasion only with no involvement inferior dental canal.
- Dentition adjacent with no periodontal ligament involvement.
This is not suitable for:
- Edentulous mandibles have alveolar bone resorption as the remaining bone is weakened and at high risk of fracture.
- Irradiated bone because the patterns of tumour spread are less predictable.
Segmental mandibulectomy
Segmental mandibulectomy is a full-thickness resection of a mandibular segmental. It can be considered in the following patients after discussion at a multidisciplinary meeting.
- Mandibular invasion regardless of patient dentition.
- Mandibular fixation in an edentulous patient.
- Mandibular hypoplasia restricts a safe rim resection.
- Carious dentition adjacent with periodontal ligament involvement.
- After radiation (radiotherapy disrupts periosteal resistance to tumour spread).
If there is an invasion of the inferior dental canal, the assumption is that there is involvement of the inferior alveolar nerve. This requires resection lateral to the lingula to medial to the mental foramen.
Types of Mandibular Reconstruction
This is guided by the defect's location and size, soft tissue loss, and dental rehabilitation. Options include no reconstruction, plates, non-vascularised bone grafts, and vascularised bone flaps.
Overview
The type of mandibular reconstruction is primarily determined by the location and size of the mandibular defect, soft tissue loss, and goals for dental rehabilitation.
Options for mandible reconstruction include no reconstruction, plates, non-vascularised bone grafts, and vascularised bone flaps.
The goals of the reconstruction should be to provide:
- Stability
- Function: opening, mastication, swallow
- Structure: dental occlusion, articulation
- Aesthetic: lower facial height and contour
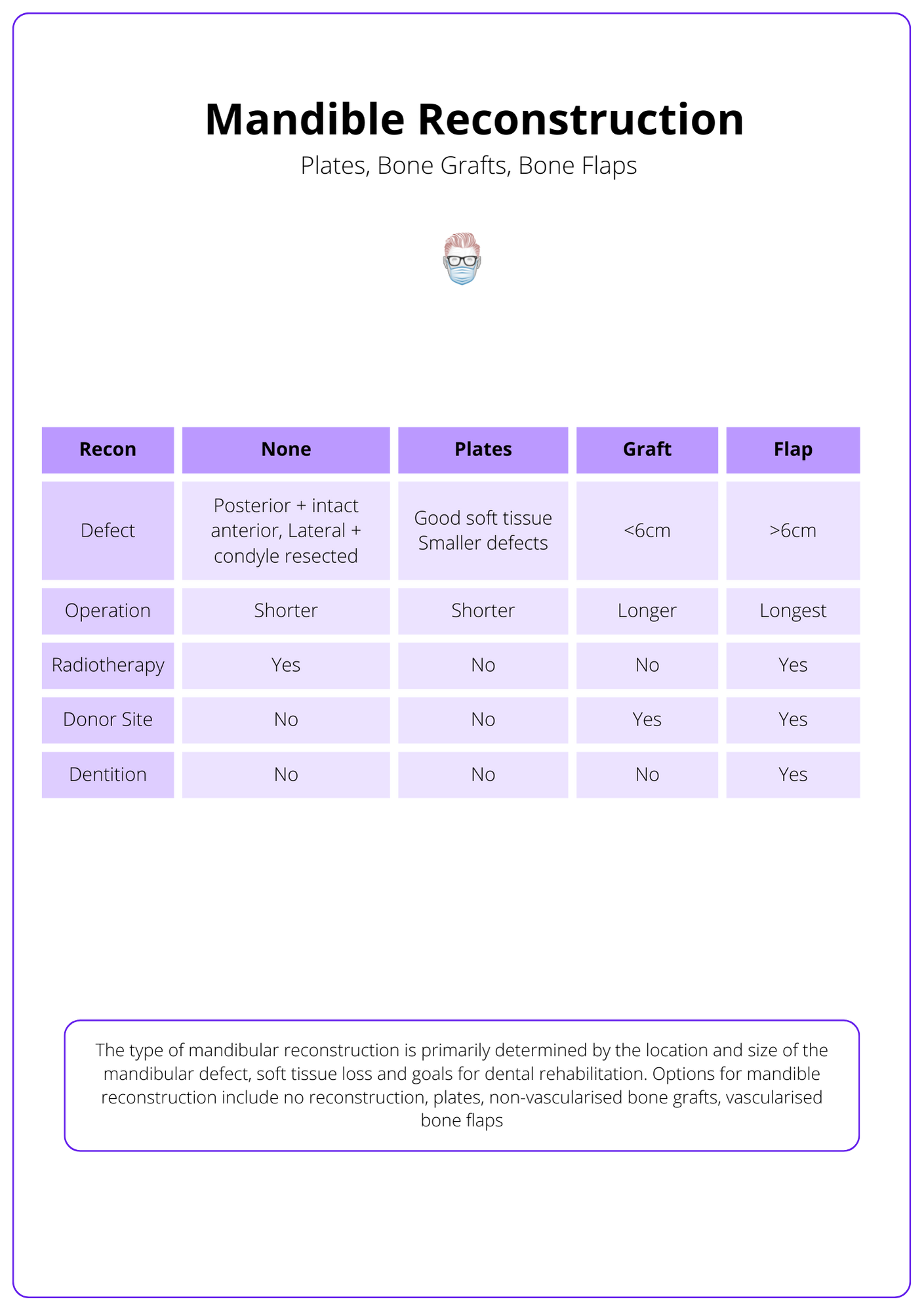
No Mandible Reconstruction
No mandible reconstruction can be considered in a select number of patients. For example:
- Indications: posterior defects with intact anterior segment, ascending ramus or lateral defects, condylar head resected from the TMJ, patient not suitable for extended operation, poor prognosis.
- Advantages: quicker operation, can usually maintain speech and swallowing.
- Disadvantages: crossbite and malocclusion.
These patients can receive soft tissue reconstruction with similar aesthetic and functional outcomes. The goal is to provide vascularized tissue bulk, obliterate dead space, and coverage of essential structures. For example, major pectoralis flap, anterolateral thigh flap, and radial artery forearm flap.
Reconstruction Plates
The operation is faster than other reconstructive options with no donor site morbidities. Mandibular plates can be considered in patients:
- Not suitable for prolonged operation.
- With a poor prognosis.
- Good soft tissue coverage.
- Not receiving radiotherapy.
This option is often complicated in the long term by:
- Plate Fracture: increased risk with radiotherapy.
- Plate Extrusion: increased risk with anterior mandible and radiotherapy.
- Stress shielding: leads to load bearing, bony resorption, and osteopenia.
- Secondary procedures to manage plate complications.
- Dental reconstruction is not possible.
- Loosening of screws.
Potential benefits include:
- Less technical.
- Shorter operation.
- No donor morbidity.
Non-Vascularised Bone Grafts
This technique requires a healthy vascularized wound bed. The graft can be taken from the rib, iliac crest, or an allograft.
Non-vascularised bone grafts can be considered for mandibular reconstruction in more minor defects (<6cm) and:
- No radiotherapy
- Not an anterior mandible defect
This reconstructive option has reduced survival with scarring, irradiation, and infection. It can be technically challenging due to inadequate skin or mucosal cover.
There is evidence to suggest this is best performed in a delayed fashion (Pogrel et al., 1997)
Vascularised Bone Flaps
Vascularised bone flaps are generally considered the gold standard in mandible reconstruction.
- Indications: Large defects (>6cm) or irradiated defects.
- Advantages: more strength and stiffness, higher arthrodesis, and superior functional outcomes compared to other reconstruction options, allowing osseointegration.
- Disadvantages: more extended operation, donor site morbidities.
Reconstruction options include:
- Free fibula flap
- DCIA flap: osteotomy possible leaving periosteum and iliacus intact, AIIS to ASIS can be used for ramus. Good vessel calibre, length, and bone height. Limited by bulkiness.
- Scapular osteocutaenous flap: low donor site morbidity, versatile as skin and bone have separate pedicles, thin bone for orbit, and hard palate. Limited by the volume of bone available and positioning.
- Radial forearm with radius: long pedicle, technically easier, thin skin can conform to any defect. Limited by quality of bone, fracture risk, and donor site problems at the wrist. More suitable for orbital reconstruction.
- MUCH less commonly used pedicled bone flaps, such as pectoralis major with 5th and 6th ribs or lateral sternum; trapezius with clavicle.
Free fibula reconstruction is improved with pre-operative mandible computer-animated drawing and modelling. Osseointegration can be planned at the same time with ProPlan 3D software - ossteintegration scews are inserted prior to elevation.
Conclusion
1. Mandibular Defect Classifications: You've gained insight into the Jewer-Boyd classification and other systems that help delineate mandibular defects, facilitating precise communication and therapeutic planning.
2. Pathophysiology of Mandibular Invasion: You now understand the mechanisms of tumor invasion of the mandible, highlighting the role of lymphatics, nerves, and the relative resistance provided by periosteum and teeth.
3. Mandibular Resections: You have become familiar with the types of mandibular resections—marginal, segmental, and hemimandibular—each with specific indications based on the extent of tumor involvement and mandibular anatomy.
4. Mandibular Reconstruction Options: You've explored various mandibular reconstruction strategies including the use of no reconstruction, reconstruction plates, non-vascularised and vascularised bone grafts, each suited to different extents of defects and patient conditions.
References
- Boyd JB, Gullane PJ, Rotstein LE, Brown DH, Irish JC. Classification of mandibular defects. Plast Reconstr Surg. 1993 Dec;92(7):1266-75. PMID: 8248401.
- Urken ML, Weinberg H, Vickery C, Buchbinder D, Lawson W, Biller HF. Oromandibular reconstruction using microvascular composite free flaps. Report of 71 cases and a new classification scheme for bony, soft-tissue, and neurologic defects. Arch Otolaryngol Head Neck Surg. 1991 Jul;117(7):733-44. doi: 10.1001/archotol.1991.01870190045010. PMID: 1863438.
- Schultz BD, Sosin M, Nam A, Mohan R, Zhang P, Khalifian S, Vranis N, Manson PN, Bojovic B, Rodriguez ED. Classification of mandible defects and algorithm for microvascular reconstruction. Plast Reconstr Surg. 2015 Apr;135(4):743e-754e. doi: 10.1097/PRS.0000000000001106. PMID: 25811586.
- Brown JS, Barry C, Ho M, Shaw R. A new classification for mandibular defects after oncological resection. Lancet Oncol. 2016 Jan;17(1):e23-30. doi: 10.1016/S1470-2045(15)00310-1. Epub 2015 Dec 23. PMID: 26758757.
- Kakarala K, Shnayder Y, Tsue TT, Girod DA. Mandibular reconstruction. Oral Oncol. 2018 Feb;77:111-117. doi: 10.1016/j.oraloncology.2017.12.020. Epub 2018 Jan 4. PMID: 29362116.
- Pogrel MA, Podlesh S, Anthony JP, Alexander J. A comparison of vascularised and nonvascularised bone grafts for reconstruction of mandibular continuity defects. J Oral Maxillofac Surg. 1997 Nov;55(11):1200-6. doi: 10.1016/s0278-2391(97)90165-8. PMID: 9371107.
- Brown JS, Lowe D, Kalavrezos N, D'Souza J, Magennis P, Woolgar J. Patterns of invasion and routes of tumor entry into the mandible by oral squamous cell carcinoma. Head Neck. 2002 Apr;24(4):370-83. doi: 10.1002/hed.10062. PMID: 11933179.


