Summary Card
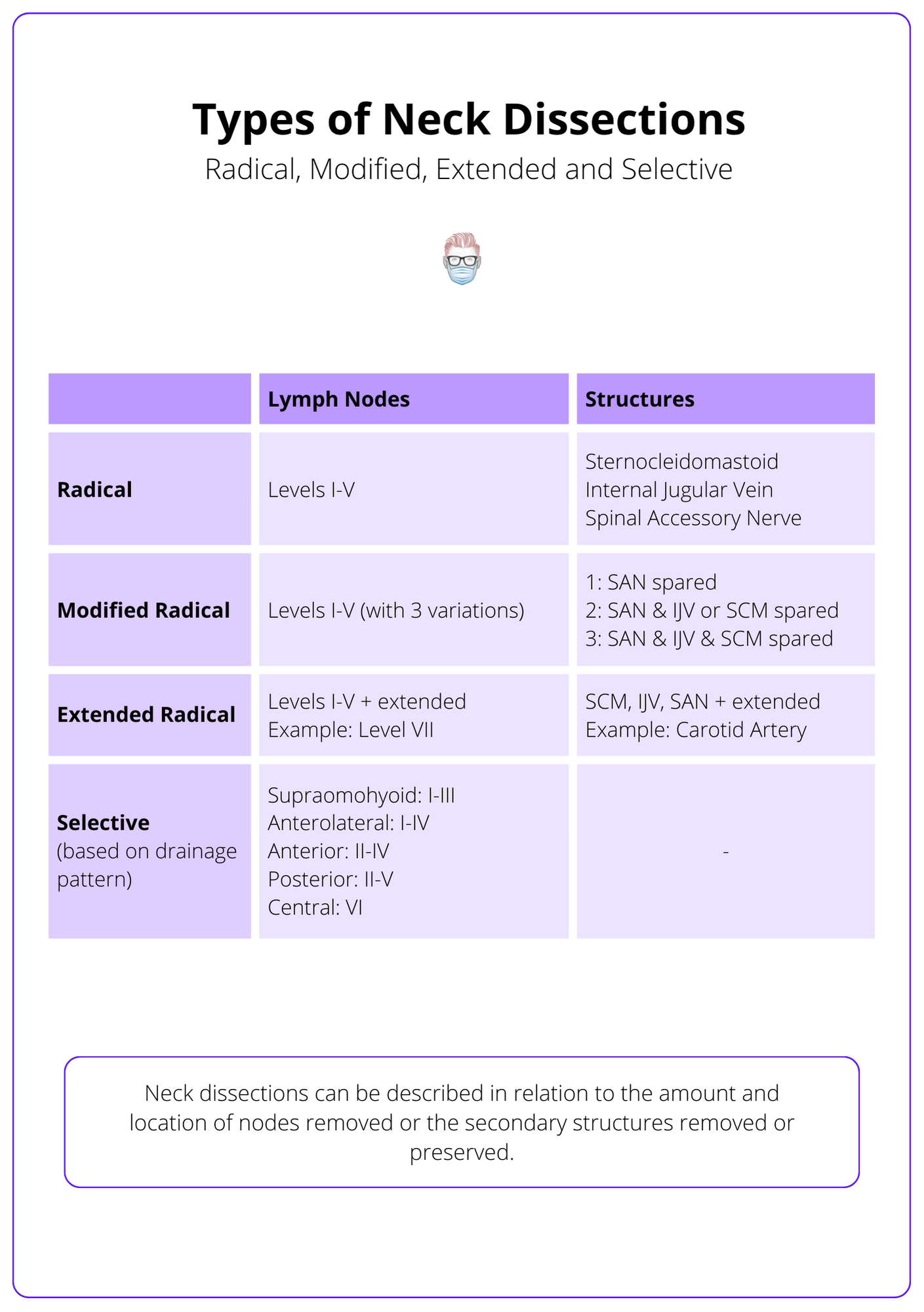
Types of Neck Dissections
"Type" refers to the location of nodes and secondary structures removed or preserved during the neck dissection.
Radical Neck Dissection
Removal of lymph nodes in levels I-V, sternocleidomastoid muscle, spinal accessory nerve, and internal jugular vein.
Modified Radical Neck Dissection
Removal of levels I-V but preserve the spinal accessory nerve and/or internal jugular vein and/or sternocleidomastoid muscle.
Selective Neck Dissection
Preserve one or more lymph node levels based on specific drainage patterns from the primary tumour site.
Indications for Neck Dissection
Selective neck dissection is indicated for node-positive cases based on N staging and node-negative cases with a high risk (>20%) of occult metastases.
Anatomy of a Neck Dissection
In a neck dissection, critical structures include the spinal accessory, marginal mandibular, vagus, hypoglossal, and more.
Neck Dissection Complications
Intra-operative and post-operative complications relating to skin, arteries, veins, nerves, and thoracic duct.
Types of Neck Dissections
Neck dissections are categorized as radical, extended, modified, or selective, based on the extent and location of lymph node removal.
Neck dissections are described as radical, extended, modified and selective. These different types of neck dissections refer to the amount and location of nodes removed or the secondary structures removed or preserved.
Types of neck dissections are illustrated in the table below.
Neck dissections can be therapeutic or prophylactic. Their indications should be discussed at a multidisciplinary meeting based on their nodal status (N1-3). Even if clinically node-negative necks (N0), there is a risk of microscopic nodal spread.
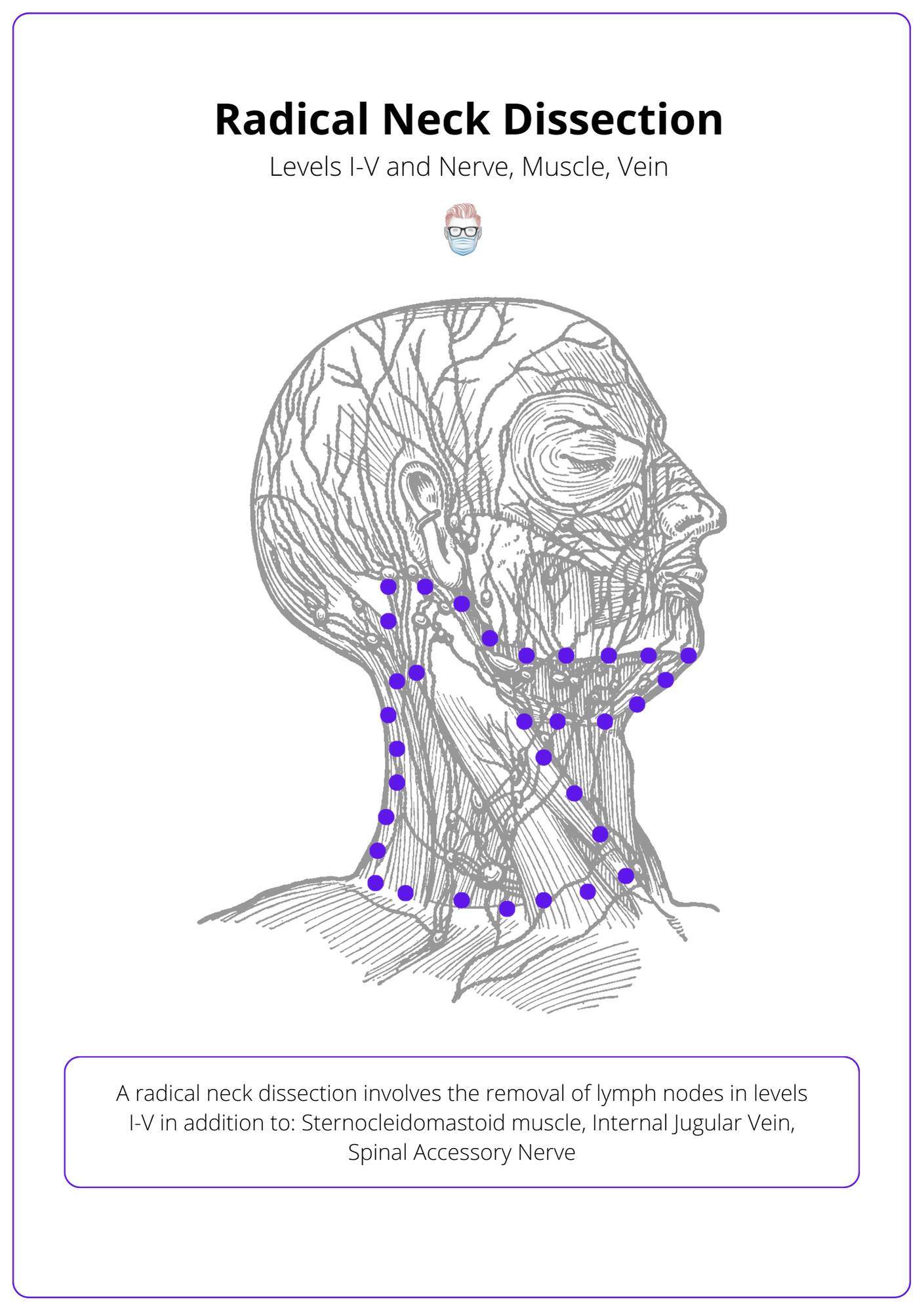
Radical Neck Dissection
A radical neck dissection involves the removal of lymph nodes in levels I-V in addition to the sternocleidomastoid muscle, spinal accessory nerve, and internal jugular vein.
The radical neck dissection was first described in 1906 by Crile, based on the Halstedian concept of en bloc resection.
A radical neck dissection involves the removal of lymph nodes in levels I-V in addition to:
- Sternocleidomastoid Muscle
- Internal Jugular Vein
- Spinal Accessory Nerve
The image below illustrates the anatomy of a radical neck dissection.
An extended radical neck dissection is the resection of lymph node groups and/or additional structures not included in the classic neck dissection.
Here is a video of a radical neck dissection (not the best audio quality, sorry!).
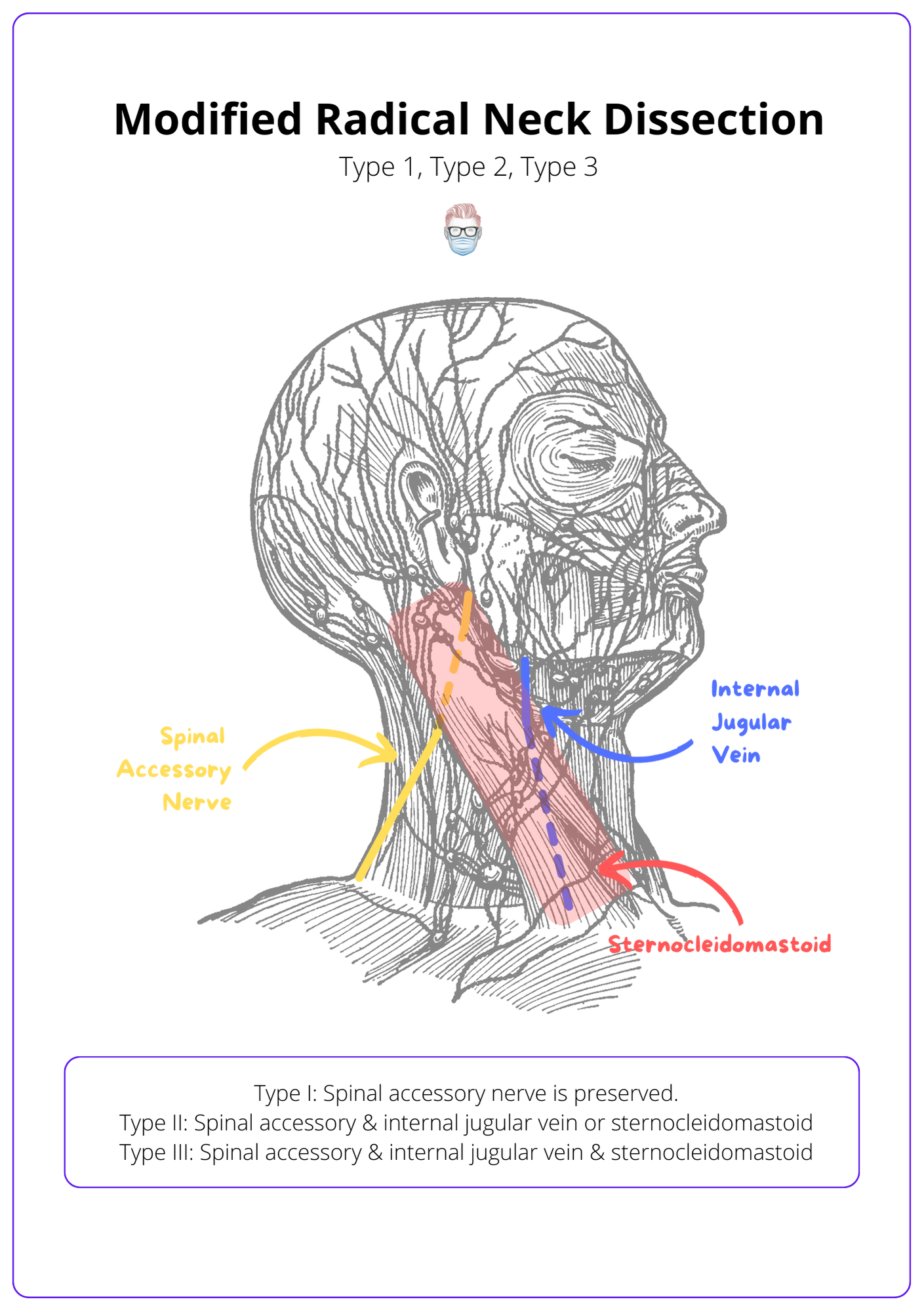
Modified Radical Neck Dissection
Modified radical neck dissections remove levels I-V but preserve the spinal accessory nerve and/or internal jugular vein and/or sternocleidomastoid muscle.
Modified radical neck dissections remove levels I-V (similar to a radical neck dissection). It is modified in the structures it preserves.
These modifications are described in relation to which structures are preserved:
- Type I: Spinal accessory nerve is preserved.
- Type II: Spinal accessory & internal jugular vein or sternocleidomastoid.
- Type III: Spinal accessory & internal jugular vein & sternocleidomastoid.
Modified radical neck dissection classification can be visualised below.
Below is an intra-operative video of a modified radical neck dissection.
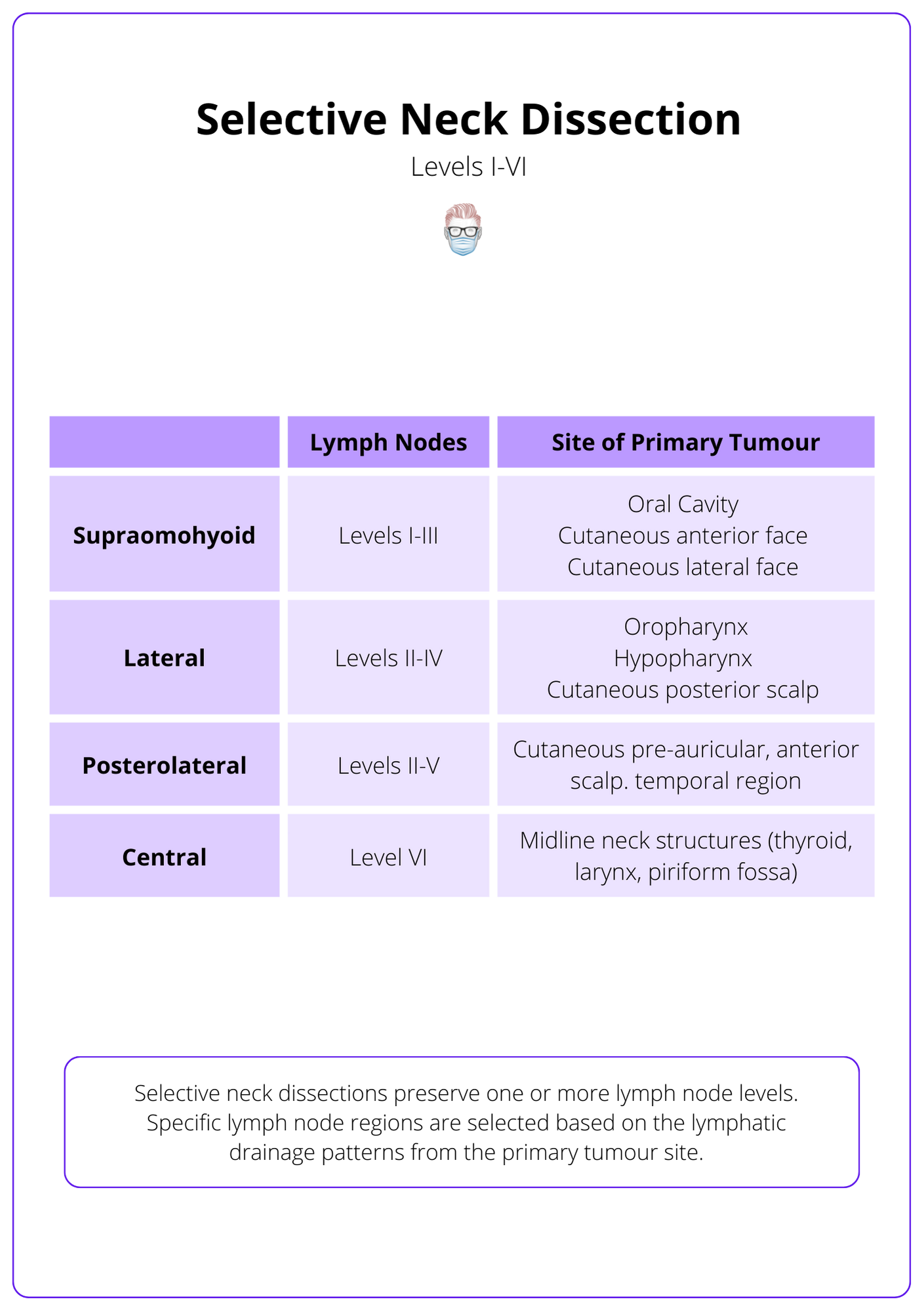
Selective Neck Dissection
Selective neck dissections preserve one or more lymph node levels based on specific drainage patterns from the primary tumour site.
Selective neck dissections preserve one or more lymph node levels. Specific lymph node regions are selected based on the lymphatic drainage patterns from the primary tumour site. Other structures are preserved (similar to a Type III modified radical neck dissection).
As illustrated in the table below, there are different types of selective neck dissections based on nodal levels removed:
- Supraomohyoid: SND I-III
- Lateral: SND II-IV
- Posterolateral: SND II-V
- Central: SND VI
The table below shows the different types of selective neck dissections.
Below is a video by the Mayo Clinic showing a selective neck dissection.
Indications for Neck Dissection
Indications for neck dissection include node-positive cases (N1-N3) and node-negative necks with >20% risk of occult metastasis.
The specific indications for a selective neck dissection should be discussed at an MDT. This operation should be considered in:
- Node-positive necks: N1 (SND), N2 (MRND III/SND), N3 (MRNDI/RND)
- Node-negative necks: risk of occult metastasis >20% (oral cavity, pharynx)
- T2 disease (varies per department and is an ongoing discussion)
Generally speaking for aerodigestive tumours:
- Oral Cavity: SND I-III (consider SND I-IV for invasive oral tumour)
- Larynx and Pharynx: SND II-IV
- Oropharyngeal: SND II-IV
- Hypopharyngeal: SND II-IV
Generally speaking for cutaneous tumours:
- Post. scalp & upper neck: SND II-V, post-auricular, suboccipital ("posterolateral SND")
- Pre-auricular, anterior scalp, temporal: SND parotid, II, III, Va and external jugular nodes ("posterolateral SND").
- Anterior and lateral face: SND parotid and facial nodes I-III
Anatomy of a Neck Dissection
Key structures in a neck dissection include the spinal accessory nerve, digastric muscle, marginal mandibular nerve, internal jugular vein, vagus nerve, hypoglossal nerve, phrenic nerve, brachial plexus, and thoracic duct.
Important structures to be aware of in a neck dissection include (and are not limited to!) the following:
- Spinal accessory nerve: travels anterior to IJV, medial to posterior digastric and stylohyoid muscles, enters SCM and exits near Erb's point (posterior border of SCM).
- Digastric muscle: travels from hyoid to mastoid tip anterior to the external and internal carotid artery, hypoglossal nerve, and internal jugular vein. The marginal mandibular nerve is lateral to the posterior belly.
- Marginal mandibular nerve: deep to the superficial layer of the deep cervical fascia and superficial to the anterior facial vein.
- Internal Jugular Vein: deep to the anterior belly of the omohyoid muscle.
- Vagus Nerve: deep to the internal jugular vein in the carotid sheath.
- Hypoglossal nerve: deep to the internal jugular vein, anterior to the internal and external carotid arteries, and continues inferior to the posterior belly of the digastric muscle to enter the tongue musculature.
- Phrenic nerve: superficial to anterior scalene muscle and deep to the transverse cervical artery.
- Brachial plexus: passes between the anterior and middle scalene muscles.
- Thoracic duct: posterior to the internal jugular vein and anterior to the phrenic and transverse cervical artery.
Neck Dissection Complications
Neck dissection complications can be intra-operative and post-operative issues relating to skin, arteries, veins, nerves, and thoracic duct.
There can be intra-operative and post-operative complications relating to the anaesthetic and the surgery itself. Specific surgical complications relevant to neck dissections include, but are not limited to:
- Soft Tissue: flap necrosis, wound breakdowns, fistula, oedema, scar contracture.
- Vessels: bleeding, embolus, stroke.
- Nerves: spinal Accessory, hypoglossal, glossopharyngeal, phrenic, plexus.
- Other: Pneumothorax, chyle leak/fistula, infections.
- Perioperatively: DVT, PE, transfusions, death.
- Radiotherapy complications (indicated in N2/N3 or extracapsular spread).
Chyle Leak in Neck Dissections
A chyle leak or fistula is a very challenging condition to treat. It is the result of damage to the left thoracic duct or the right lymphatic duct. It presents as a collection or milky discharge.
Diagnosis can be made by testing drain triglyceride levels greater than serum levels, absolute drain triglyceride levels greater than 100 mg/dL, or with the presence of chylomicrons.
Treatment options include:
- Fat-free diet or medium-chain diet to reduce the volume of the leak.
- Total Parenteral Nutrition may be required.
- Consider octreotide.
- Gradually reduce suction off the drain.
- If exploration is required (rare), consider a sternocleidomastoid flap turnover.
- Thoracoscopic ligation of ductal tissue as it travels through the diaphragmatic hiatus between the azygous vein and the aorta.
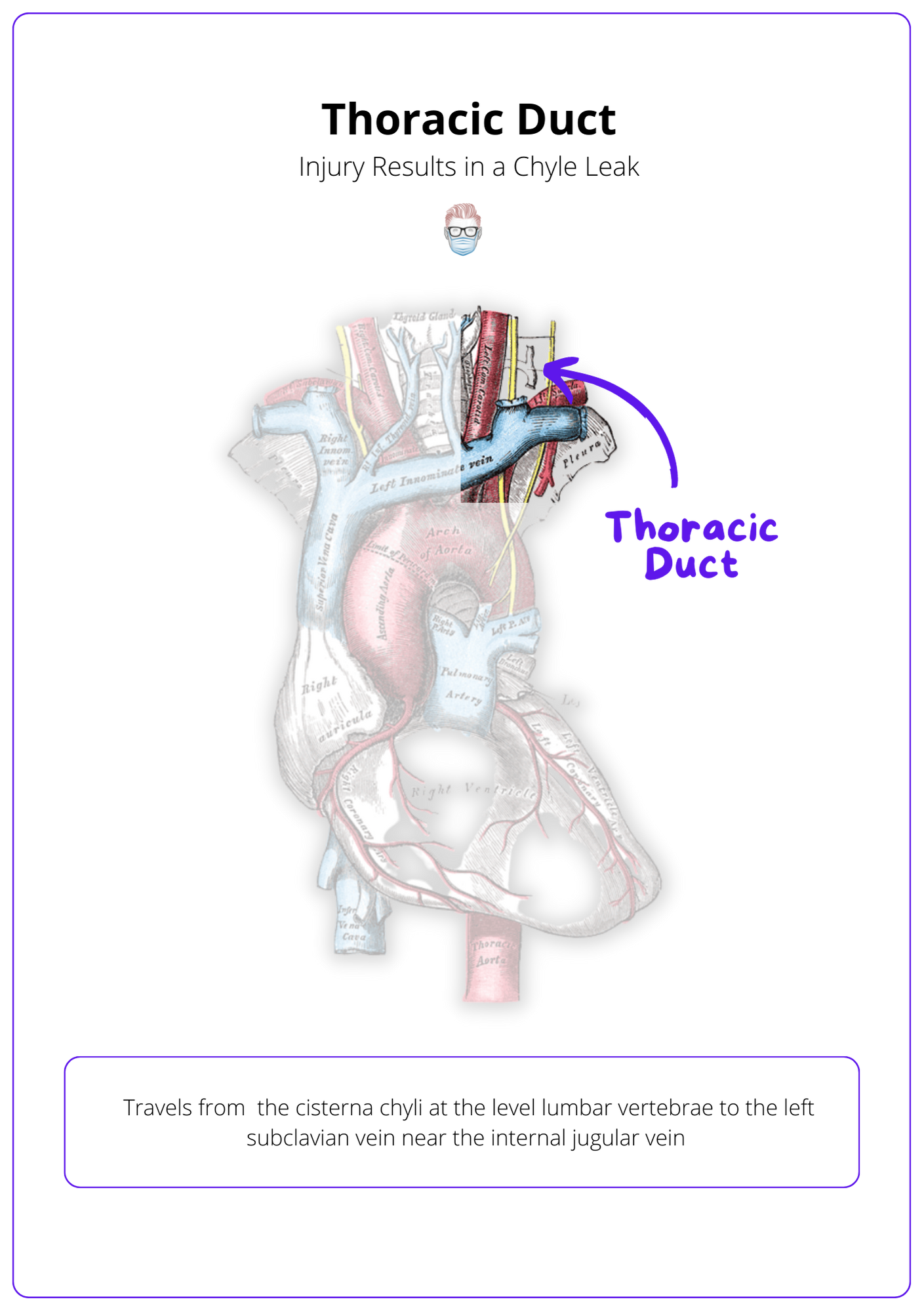
There are some significant anatomical variations in the left thoracic duct, but generally speaking:
- Starts from the cisterna chyli at the level of lumbar vertebrae.
- Via aortic hiatus, posterior mediastinum, oesophagus, over the subclavian artery.
- Finishes at the left subclavian vein near the internal jugular vein.
The image below illustrates the thoracic duct.
Conclusion
1. Types of Neck Dissections: You've gained knowledge about the various types of neck dissections — radical, modified radical, and selective — and their specific applications based on the extent of lymph node removal and the preservation of key anatomical structures.
2. Neck Dissection Indications: You are now familiar with the criteria for selecting the appropriate type of neck dissection based on nodal involvement and the likelihood of occult metastases for surgical planning.
3. Anatomical Considerations: You've learned about the critical anatomical landmarks and structures involved in neck dissections, vital for minimizing complications and ensuring effective surgical outcomes.
4. Awareness of Complications: You understand the potential intra-operative and post-operative complications associated with neck dissections, including risks to specific nerves, vascular structures, and other tissues for patient management and counseling.
5. Management Strategies for Complications: You've explored the management strategies for specific complications such as chyle leaks to optimize patient recovery and outcomes.


