Summary Card
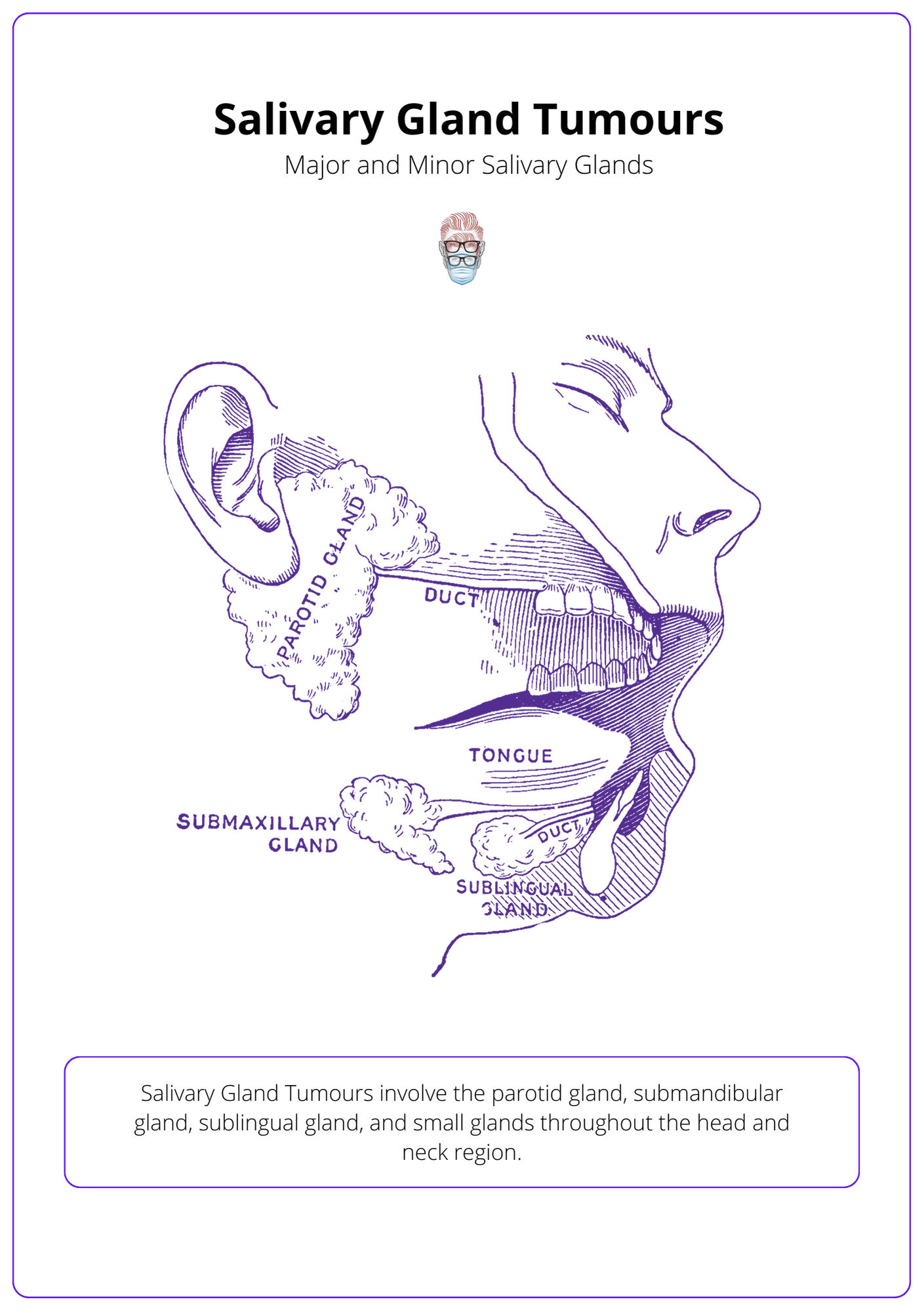
Anatomy of Salivary Gland Tumours
The parotid, submandibular, sublingual, and minor salivary glands have unique anatomy and duct systems.
Classification of Salivary Gland Tumours
By location (parotid, submandibular, sublingual or minor glands) and by pathology (benign or malignant).
Benign Salivary Gland Tumours
The commonest type of salivary gland tumours. Pleomorphic adenoma is the most common, followed by Warthin's Tumour.
Malignant Salivary Gland Tumours
They can be primary or secondary. The most common is mucoepidermoid carcinoma in the parotid gland.
Investigations of Salivary Gland Tumours
Ultrasound with fine-needle aspiration for cytology. CT or MRI can be considered for anatomical delineation and staging.
Anatomy of Salivary Gland Tumours
The salivary glands consist of parotid, submandibular, sublingual and minor salivary glands.
The "salivary glands" develop during weeks 6-8 of gestation to form the parotid, submandibular, sublingual and minor salivary glands.
Parotid:
- Serous acini primarily.
- deep and superficial lobes separated by the facial nerve, and tail.
- Surrounding fascia is a continuation of deep cervical fascia.
- Stensen's duct: anterior border to 2nd maxillary molar.
Submandibular
- In submandibular triangle.
- Mucous & Serous Acini.
- Wharton’s Duct into the anterior floor of the mouth.
Sublingual
- In the anterior floor of the mouth.
- Multiple ducts of Rivinus form Bartholin's duct, which empties into Wharton's duct.
Minor glands
- Common locations include labial, buccal, palatine, anterior and posterior lingual. There are over 600 - 1000.
- Mainly mucous secreting.
Classification of Salivary Gland Tumours
Salivary gland tumours can be classified by their location (parotid, submandibular, sublingual, or minor glands) and by their pathology (benign or malignant).
Salivary gland tumours can arise from epithelial, mesenchymal and lymphoid tissue.
The major and minor salivary glands are associated with a remarkable diversity of neoplasms. WHO histologic classification for salivary gland tumours has over 40 different types of tumours as they can arise from epithelial, mesenchymal and lymphoid tissues. There were recent updates in their 8th edition publication on Salivary Gland Tumours.
The image below illustrates major and minor salivary glands and the location of salivary gland tumours.
From a clinical perspective, salivary gland tumours can be classified by the type of gland and their degree of malignancy.
Type of Gland
The most common location of a salivary gland tumour is the parotid gland but it does have the least risk of malignancy.
- Major salivary gland: parotid, submandibular, sublingual.
- Minor salivary gland: small glands throughout the head and neck region.
Disease
These are just some examples of the 40+ different types of salivary gland tumours.
- Benign: pleomorphic adenoma, adenolymphoma, oncocytoma, sebaceous neoplasms, intraductal papilloma.
- Benign Soft Tissue: Haemangioma (commonest paediatric salivary gland tumours), Lipoma, sialolipoma, nodular fasciitis.
- Malignant: mucoepidermoid, adenoid cystic, acinic cell, mixed, adenocarcinoma (from myoepithelium), primary SCC, sebaceous, lymphoma.
- Non-neoplastic epithelial: sclerosing polycystic adenosis, nodular oncocytic hyperplasia, lymphoepithelial sialadenitis, intercalated duct hyperplasia.
- Hematolymphoid: mucosa-associated lymphoid tissue (MALT lymphoma).
Benign Salivary Gland Tumours
Benign tumours are the most common type of salivary gland tumours. Pleomorphic adenoma is the most common in adults and children, followed by Warthin's Tumour.
Benign tumours are the most common type of salivary gland tumours. The two most frequently diagnosed are pleomorphic adenoma (commonest solid tumour in children) and adenolymphoma. Less common benign tumours include intraductal papilloma, sebaceous neoplasms and oncocytoma.
Typically, they present as a painless, slow-growing mass. There are several different types, and here are some examples below.
Pleomorphic Adenoma
- Incidence: most common salivary tumour & often in middle-aged females.
- Pathology: benign mixed tumour with a low malignant potential (~10%).
- Location: often parotid (esp. superficial lobe tail), less likely submandibular.
- Surgery: superficial parotidectomy or total parotidectomy if deep lobe with facial nerve preservation or total resection of a non-parotid salivary gland resection. Tumour is not encapsulated, which means simple enucleation would result in high recurrence rates.
- Radiotherapy: No role for radiotherapy.
Adenolymphoma (Warthin's Tumour)
This condition can also be referred to as papillary cystadenoma lymphomatosum.
- Incidence: ~20% of salivary tumours & often in middle-aged smoking males.
- Pathology: epithelial and lymphoid components with abundant cystic spaces.
- Location: nearly always in the parotid, ~10% are bilateral & multicentric.
- Treatment: superficial or deep parotidectomy with facial nerve preservation.
Malignant Salivary Gland Tumours
Malignant salivary gland tumours can be primary or secondary. The commonest is mucoepidermoid carcinoma in the parotid gland.
Malignant salivary gland tumours can be primary or secondary malignancies (less common) with different histopathological grades (high, low or mixed). They are most commonly found in the parotid gland and less so in the submandibular gland.
Clinical features of salivary gland malignancy include pain, facial nerve palsy, rapid growth, obstructive symptoms or local invasion.
The most common salivary gland tumours are mucoepidermoid carcinoma (also in children), followed by adenoid cystic carcinoma and acinic cell carcinoma. Less common malignancies include adenocarcinoma, primary SCC, sebaceous carcinoma and lymphoma.
Mucoepidermoid Carcinoma
- Incidence: commonest parotid malignancy, middle-aged males & females.
- Pathology: variable malignant potential based on histological grade, contains mucus-secreting cells, and epithelial cells of the epidermoid variety. It arises from the excretory duct.
- Location: usually in the superficial lobe of the parotid.
- Treatment: consider adjuvant radiotherapy, parotidectomy, neck dissection.
Adenoid Cystic Carcinoma
This is the most common malignancy of the sublingual, submandibular and minor salivary glands (mucoepidermoid carcinoma is the second most common).
- Incidence: in middle-aged and elderly males and females.
- Pathology: cribriform (Swiss-cheese, better prognosis), tubular (low grade), solid (high grade). It arises from the intercalated duct.
- Location: usually in the submandibular gland.
- Treatment: adjuvant radiotherapy, resection, high recurrence risk.
Acinic Cell Carcinoma
- Incidence: in middle-aged patients.
- Pathology: usually a low-grade multifocal tumour (once considered benign!) arising from the acinus.
- Location: occurs most often in the parotid gland.
- Treatment: Total parotidectomy; radiotherapy has no role.
Investigations of Salivary Gland Tumours
After a history and examination, an ultrasound with fine-needle aspiration for cytology should be performed. CT or MRI should be considered for anatomical delineation and staging.
The diagnosis of salivary gland tumours is based on history, examination findings and investigative results. Investigations to consider are:
- Fine Needle Aspiration for Cytology: benign vs malignant.
- Ultrasound: guides FNAC, assess location and lymph nodes.
- CT or MRI: anatomical location, staging for metastasis.
- Open Biopsy: can cause tumour seeding.
A differential diagnosis for a parotid gland swelling can include the aforementioned benign and malignant tumours, and also:
- Sialadenitis: chronic swelling independent of eating.
- Sialolithiasis: recurrent pain and swelling with eating. It is the most common cause of submandibular swelling and can be diagnosed with a Sialogram.
- Granulomatous disease: sarcoid, actinomycosis, mycobacterium.
- Transient glandular hypertrophy (bulimics).
AJCC Staging
- T1: <2 cm without extraparenchymal extension.
- T2: 2-4 cm without extraparenchymal extension.
- T3: >4 cm and/or having extraparenchymal extension.
- T4: >6 cm or extension into extraglandular tissues.
- T4a: Invades skin, mandible, ear canal, or facial nerve.
- T4b: Invades skull base, pterygoid plates, carotid artery.
Neck dissection is indicated for malignant salivary gland tumours with clinically positive nodes detected either on physical examination or with preoperative imaging workup.
Conclusion
1. Anatomy of Salivary Glands: You've learned about the structural intricacies of the major and minor salivary glands, including their acini types, ductal systems, and anatomical positions, essential for understanding disease processes and surgical approaches.
2. Salivary Gland Tumour Classifications: You now have insight into how salivary gland tumours are classified based on their location and pathology, aiding in accurate diagnosis and tailored treatment planning.
3. Benign Salivary Gland Tumours: You've explored the most common types of benign tumours, such as pleomorphic adenoma and Warthin's tumour, including their typical presentations and treatment options, enhancing your ability to manage these conditions effectively.
4. Malignant Salivary Gland Tumours: You've examined the characteristics of malignant salivary gland tumours, including common types like mucoepidermoid carcinoma, and their implications for prognosis and therapy.
5. Diagnostic Investigations for Salivary Gland Tumours: You are now familiar with the key investigative techniques used in the diagnosis of salivary gland tumours, such as ultrasound-guided fine-needle aspiration, CT, MRI, and the importance of staging in treatment planning.