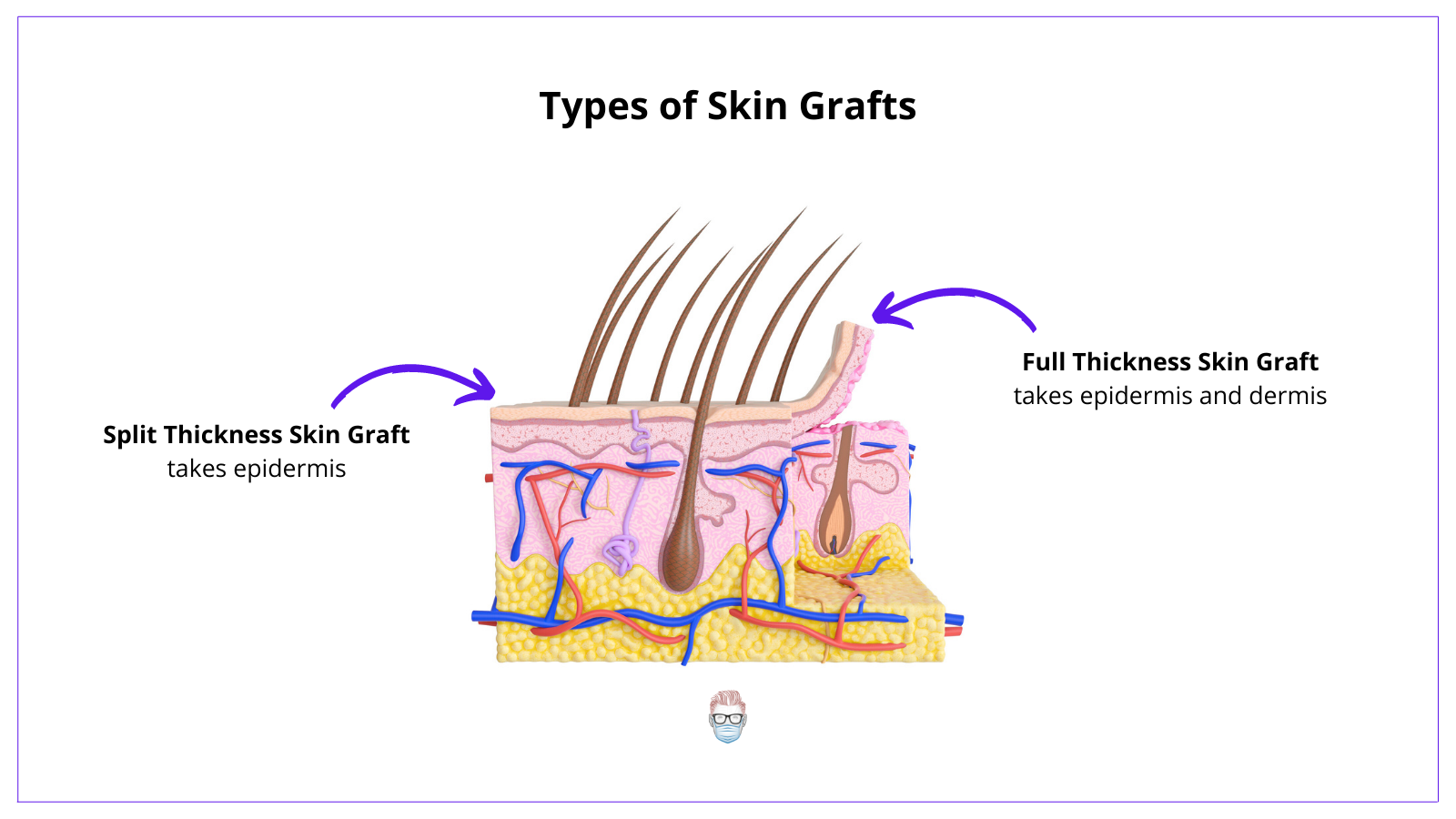
Types of Skin Grafts
A skin graft can be a "full-thickness skin graft" or a "split-thickness skin graft".
- Full-thickness skin grafts contain epidermis and dermis
- Split thickness skin grafts contain epidermis and variable amounts of dermis.
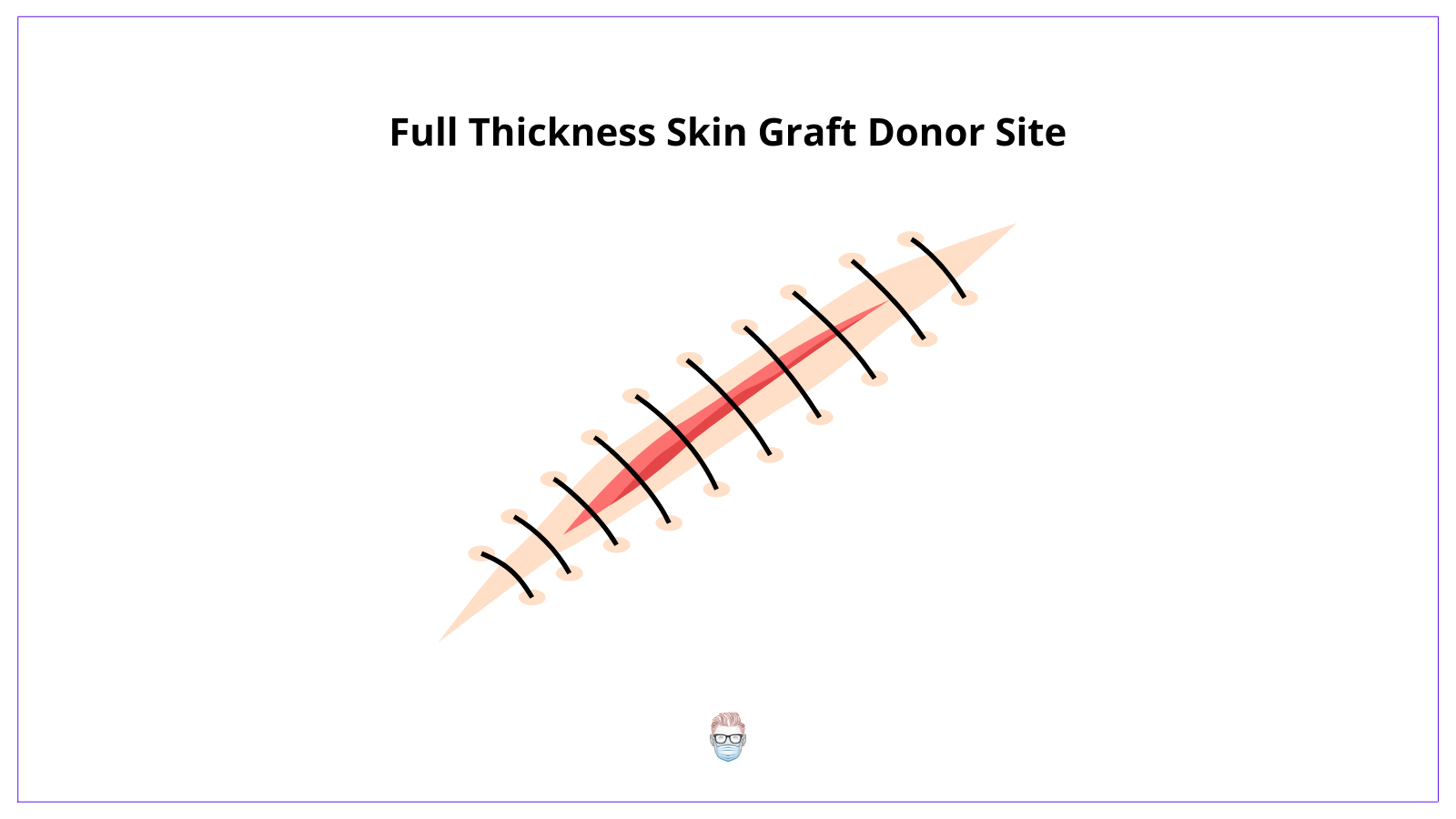
Skin Graft Donor Sites
Full-thickness are taken from areas that can close primarily and have a good colour match to the defect. For example, a pre-auricular or a supraclavicular donor site for defect reconstruction to the nose.
Split thickness skin grafts are often taken from the lateral thigh or buttock. They heal by re-epithelialisation. This is because there are adnexal remnants left at the donor site.

Stages of Skin Graft Healing
Stages of Skin Graft Healing
A skin graft healing process is often described as "skin graft take". This healing process requires skin graft adherence, imbibition, revascularisation and remodelling. This is detailed below in the image.
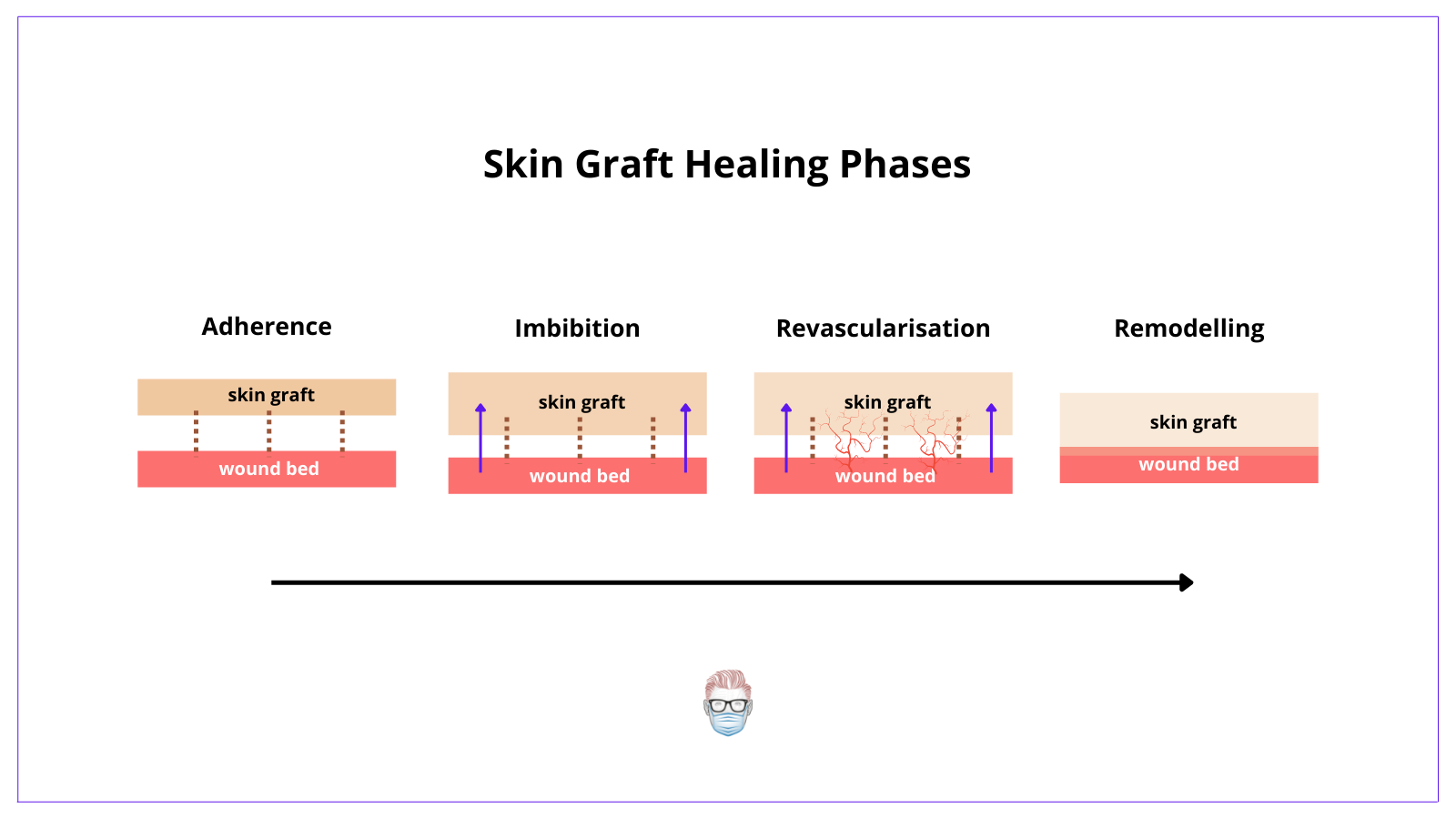
1. Skin graft adherence
- This occurs instantly if a suitable bed has been selected for the skin graft
- Fibrin bonds form and the proliferation of fibroblasts replace the fibrin with collagen.
2. Serum Imbibition
- The graft absorbs fluids within 72 hours resulting in increased graft size
- The fluid contains nutrition to keep the graft viable.
3. Revascularisation
- A small vascular network starts to form in the fibrin layer connected to the graft and the wound bed after ~72 hours.
- This occurs through inosculation and neovascularization which allow the outgrowth of capillary buds.
- This brings "pinkness" to the graft.
4. Remodelling
- Graft architecture returns to "normal skin"
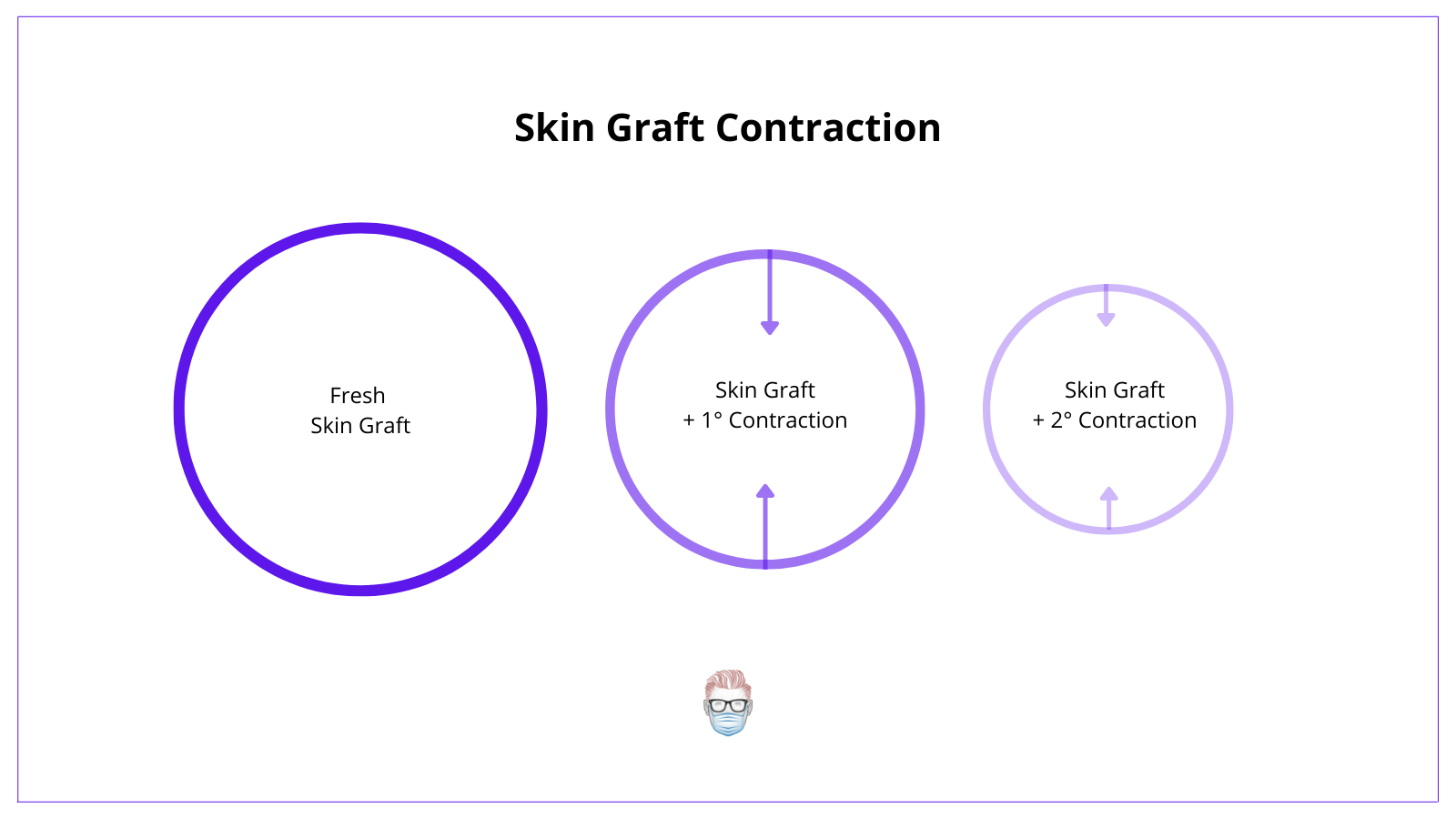
Skin Graft Contraction
Skin grafts undergo primary and secondary contraction. It is influenced by the degree of the dermis (and its elastin) and the thickness of the skin graft.
- Primary contraction is the immediate recoil of the skin graft that occurs more markedly in full-thickness skin grafts.
- Secondary contraction occurs after the skin graft healing process and is more common in split-thickness skin grafts.
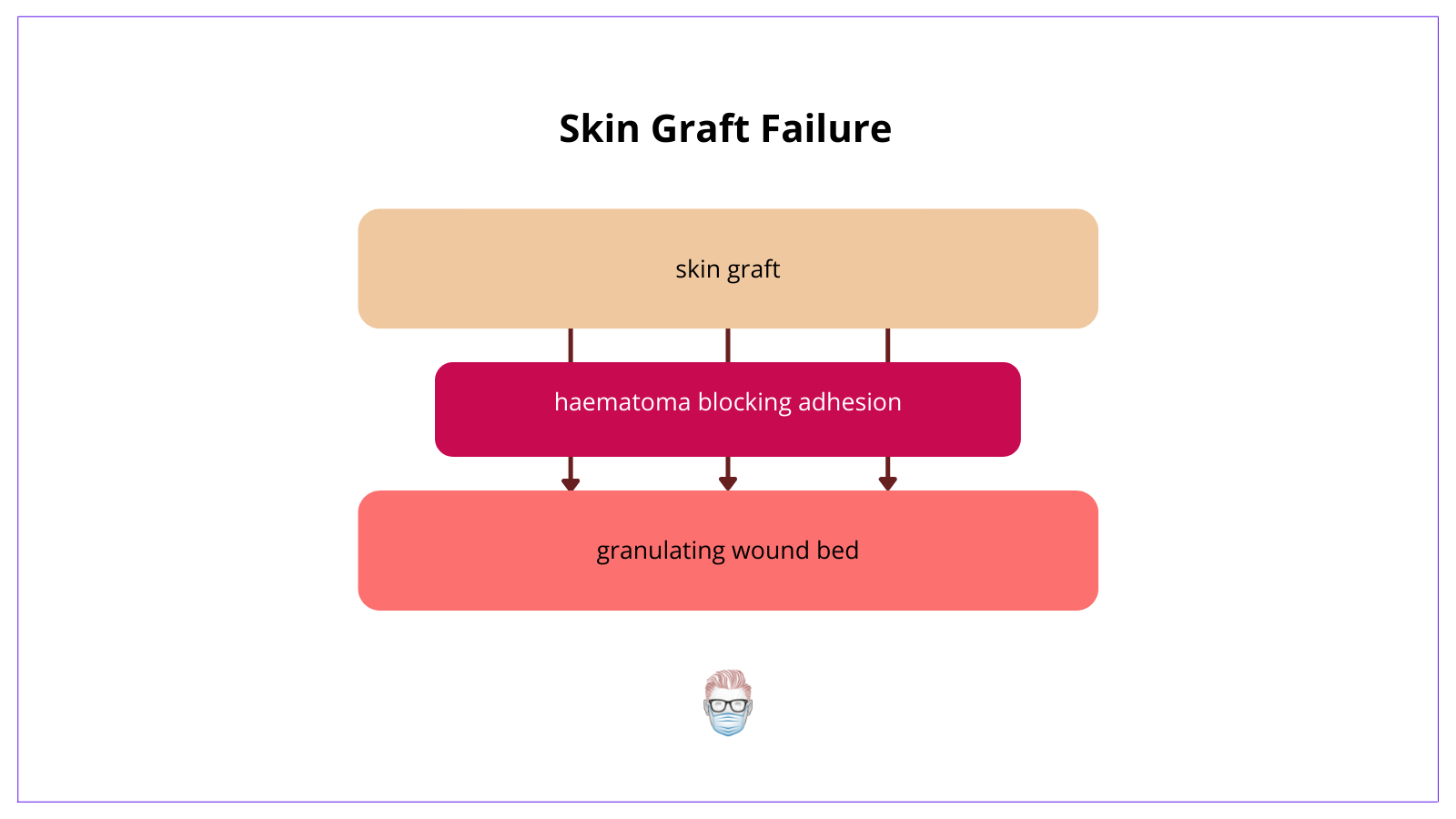
Skin Graft Failure
Skin graft failure is a relatively uncommon event. Here are some reasons for failure
- Infection: group A B-haem Strep (Strep Pyogenase) secretes proteases which prevent adherence.
- Haematoma prevents adherence (reduce risk by meshing the skin graft!)
- Shearing Forces (a fancy way of saying lateral forces) disrupt adherence.
- Wound Bed: skin grafts require a blood supply (not good on bone or tendon)
In certain cases, a skin graft can survive by a phenomenon called "bridging". This can occur if a graft is separated from its wound bed or overlying a non-vascular structure. The graft can link up with an existing vascular network.


