5 Key Points on Wound Healing
1. Types of Wound Healing
Wound Healing can be via primary, secondary or tertiary intention
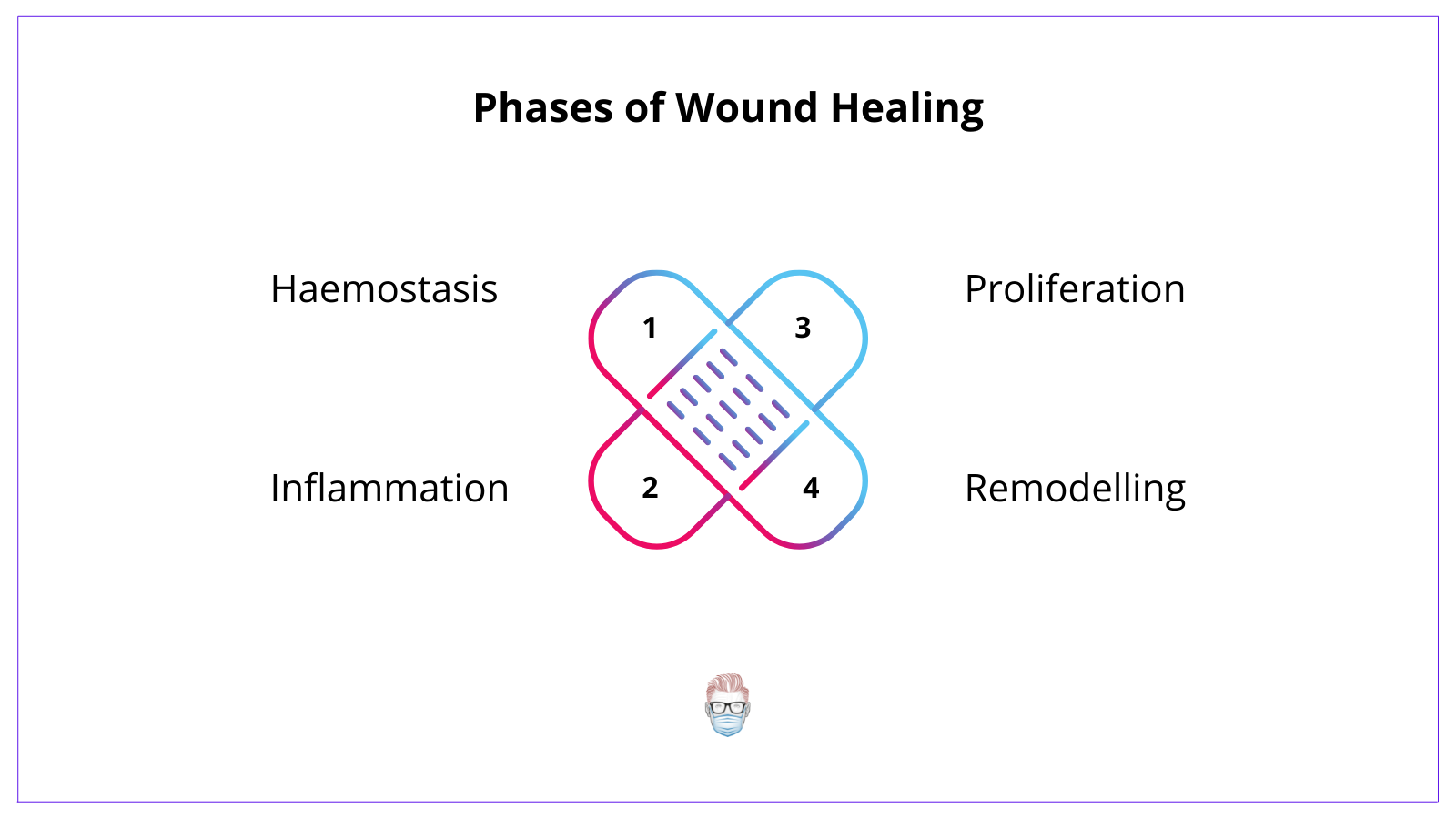
2. Phases of Wound Healing
Phases of wound healing are hemostasis, inflammation, proliferation and remodelling.
3. Important cells in wound healing
Macrophages, neutrophils and fibroblasts play integral roles in activating pathways, reducing bacterial burden, and promoting collagen formation, respectively.
4. Re-epithelialisation vs Contraction
Re-epithelialisation occurs in wounds with an intact epidermal basement membrane via mobilisation, migration, mitosis and differentiation.
Contraction occurs in wounds after 3 days and is caused by myofibroblasts.
5. Factors affecting healing
There are genetic conditions, acquired systemic issues and local factors that all influence wound healing.
Types of Wound Healing
There are 3 ways a wound can heal:
- Primary closure: most common
- Secondary intention: open wound that granulates, contracts, epithelialises
- Tertiary Intention: delayed primary (a wound that is closed at a later date)
Here is an in-depth video tutorial.
Phases of Wound Healing
1. Haemostasis
This occurs acutely and is initiated once a wound has been created.
The key aspects of this include:
- Vasoconstriction from thromboxane & prostaglandins release.
- Activating platelet-activating factor, von Willebrand, & thromboxane A2.
- Platelet plug formation secondary to platelet activation
- Thrombus formation is secondary to fibrinogen converted to fibrin. This can weakly hold the wound together.
2. Inflammation
This occurs within the first 72 hours of the initial activation of the wound healing pathway.
The key aspects of this include:
- Cell proliferation is secondary to the release of platelet-derived growth factors and pro-inflammatory factors (serotonin, bradykinin, histamine).
- Vasodilation as endothelial cells swells and polymorphonuclear neutrophils travel into the tissue.
- Cellular immunity and antibody production from T-lymphocytes entering the wound (influence by interleukin-1) and secreting cytokines.
3. Proliferation
This occurs after ~72 hours and is usually complete within 2-4 weeks.
The key aspects of this include:
- Matrix formation from fibroblasts & glycosaminoglycan production.
- Collagen & elastin production is secondary to fibroblasts (mainly type III). This can hold the wound together quite strongly.
- Wound contraction as fibroblasts differentiates into myofibroblasts.
- Angiogenesis secondary to endothelial stem cell migration. This is assisted by macrophages stimulating nearby vascular endothelium of adjacent capillaries.
4. Remodelling
This occurs after 2-4 weeks from injury and can last >1 year. This phase of wound healing is responsible for the tensile strength of a wound.
The key aspects of this include:
- Collagen Haemostasis: no increase in collagen production
- Collagen replacement: type III collagen is replaced by type I (stronger).
- Collagen re-organisation: becomes organised with stronger cross-links.
- Apoptosis removes the capillary network and creates a pale-looking scar.
The type of cell involved in wound healing changes over time. The first cells are predominantly neutrophils. After 48 hours, macrophages become dominant during the inflammatory phase. Fibroblasts and myofibroblasts play an important role in proliferation and remodelling.
Re-epithelialisation in Wound Healing
Re-epithelialisation occurs after the basement membrane of the epidermis has been breached. It occurs from the edges of the wound and epidermal appendages.
The 4 phases of re-epithelialisation are as follows:
- Mobilisation: epithelial cells lose contact with neighbours (contact inhibition) to become flat and long and form pseudopodia.
- Migration: epithelial cells attempt to overcome contact inhibition by moving centrally.
- Mitosis: epithelial cells proliferate once, desmosomes and hemidesmosomes attach to the basement membrane and form a stratum germinativum.
- Differentiation: cells differentiate to recreate normal stratified squamous epithelium.
Contraction in Wound Healing
Contraction is a normal phenomenon in a granulating wound bed due to myofibroblasts. Here are some key points on myofibroblasts
- First appear ~72 hours after injury and peak at 2-3 weeks.
- Contain contractile microfilaments and distinct cellular adhesions (desmosomes and maculae adherens)
- Disappear when contraction is complete
Wound Healing Factors
Medical conditions
The following medical conditions negatively influence the ability of a wound to heal:
- Pseudoxanthoma elasticum: increased collagen degradation giving a pebble-skin appearance.
- Epidermolysis Bullosa: skin is very delicate
- Ehler's Danlos Syndrome: abnormal collage structure
- Cutis Laxa: mutated elastic fibres presenting in newborns as excessive laxity.
- Werner Syndrome: mutated WRN gene presenting similarly to scleroderma.
- Progeria: mutated LMNA gene creating an appearance of "premature ageing".
Systemic Factors
The following systemic factors play an important role in wound healing.
- Age: as you age so too does your ability for cell re-growth and tensile strength.
- Smoking: nicotine induces vasoconstriction, carbon monoxide decreases oxygen-carry capacity, and hydrogen cyanide impairs oxygen transport
- Comorbidities: for example diabetes.
- Nutrition: vitamin A (retinol) and C are required for collagen cross-linking and synthesis, respectively. Vitamin E stabilises the membrane. Low albumin is a predictor of poor wound healing.
- Medication: steroids inhibit epithelialisation & decrease collagen production.
Local Wound Factors
Local wound issues are usually the most common reason for delayed wound healing. It can relate to:
- Infection: reduces oxygen tension, pH, epithelialisation and angiogenesis, whilst increasing collagenase activity and inflammation
- Radiation: occludes small vessels, and damages fibroblasts and nuclei.
- Temperature: warm and moist increase epithelialisation and tensile strength.
- Oxygen delivery: microvascular disease results in reduced tissue perfusion.
Flashcards
They are continually updated and are for thePlasticsPro users.
This is for thePlasticsPro
Join the Club to enjoy unlimited access to all of thePlasticsFella.
Join the Club

