Summary Card
Hard Palate
Maxilla and palatine bones are covered by 3 mucosal zones with 3 portals (incisive, greater and lesser palatine).
Soft Palate
5 paired muscles are innervated by the pharyngeal plexus and trigeminal nerve.
Neurovascular Supply
Primarily by the greater palatine artery and nerve, and the lesser palatine artery and nerve.
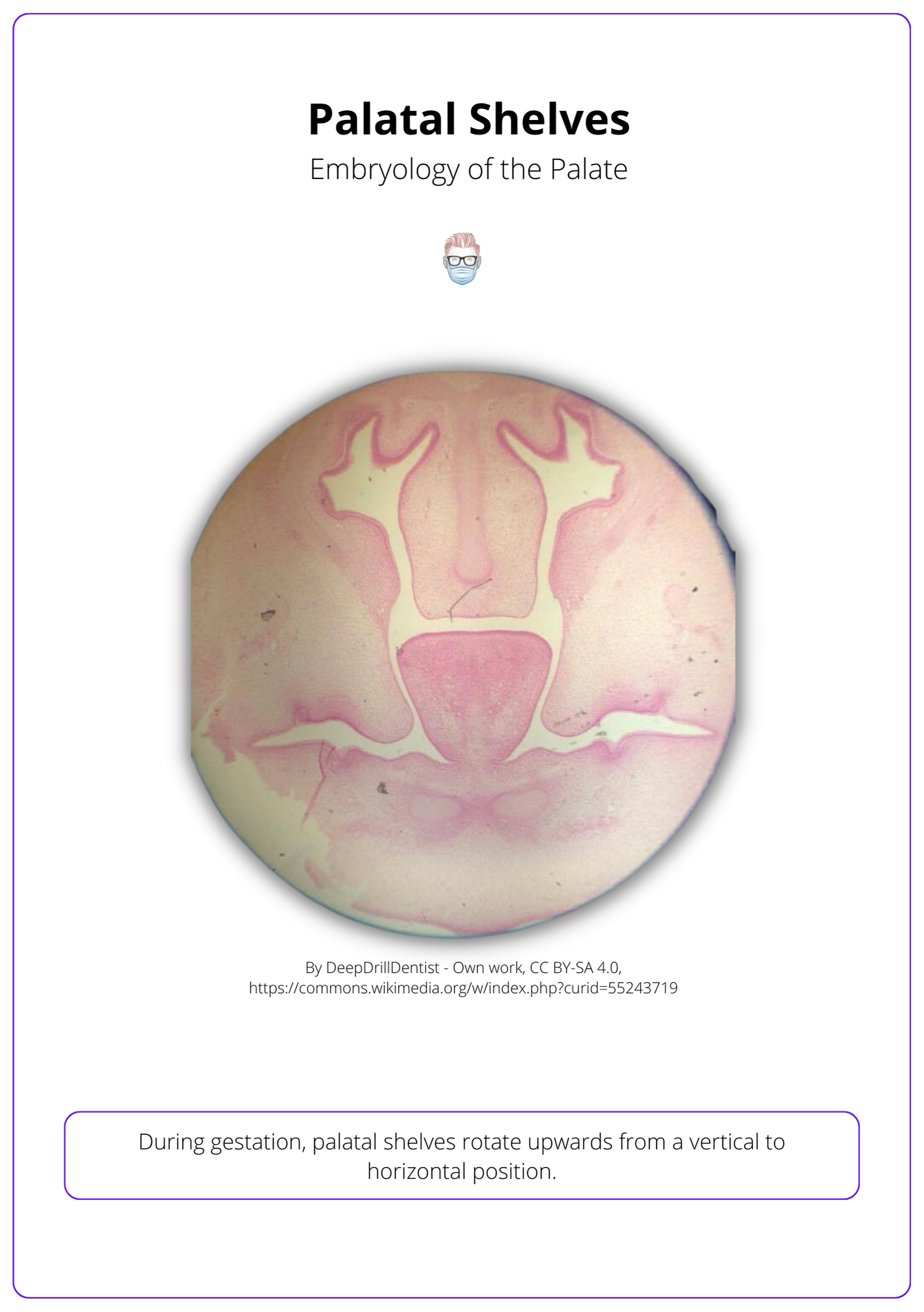
Embryology of the Palate
Palate forms during the second month of gestation as the mandible grows, the tongue descends and shelves turn horizontal.
Cleft Palate Anatomy
A spectrum of abnormal muscular and bony anatomy relating to the hard and soft palate.
Hard Palate
The hard palate is formed by the maxilla and palatine bones. It is covered by 3 mucosal zones and has 3 portals (incisive, greater and lesser palatine).
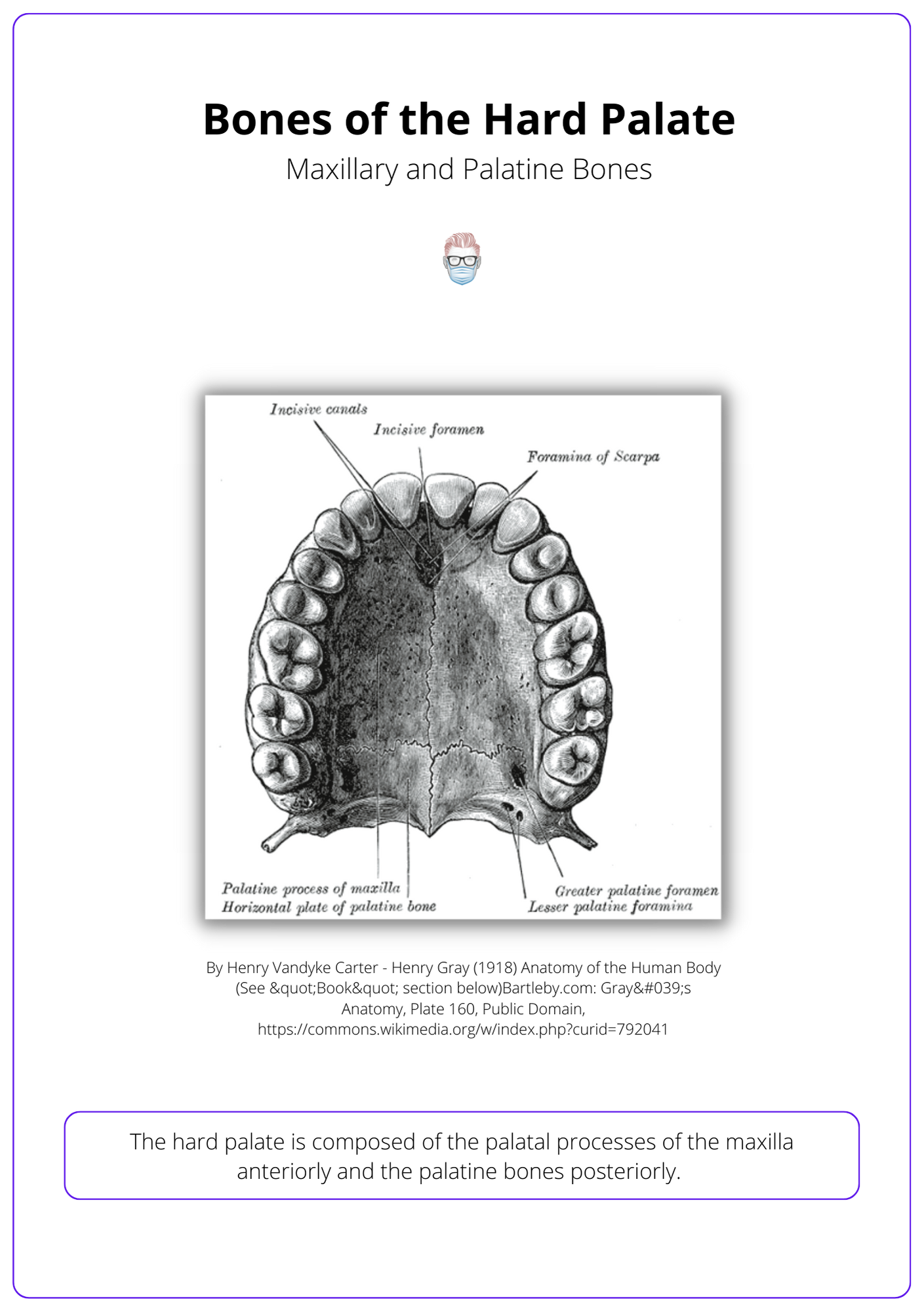
Bones
The primary and secondary hard palate is created by 2 bones: maxilla and palatine.
- Primary palate is anterior to the incisive foramen and is formed by the lip, nostril sill, alveolus, premaxillary portion of the maxilla.
- Secondary palate is posterior to the incisive foramen and is formed by the palatal processes of maxilla (anterior), palatine bone (posterior) and soft palate.
These hard palate bones are visualised in the image below.
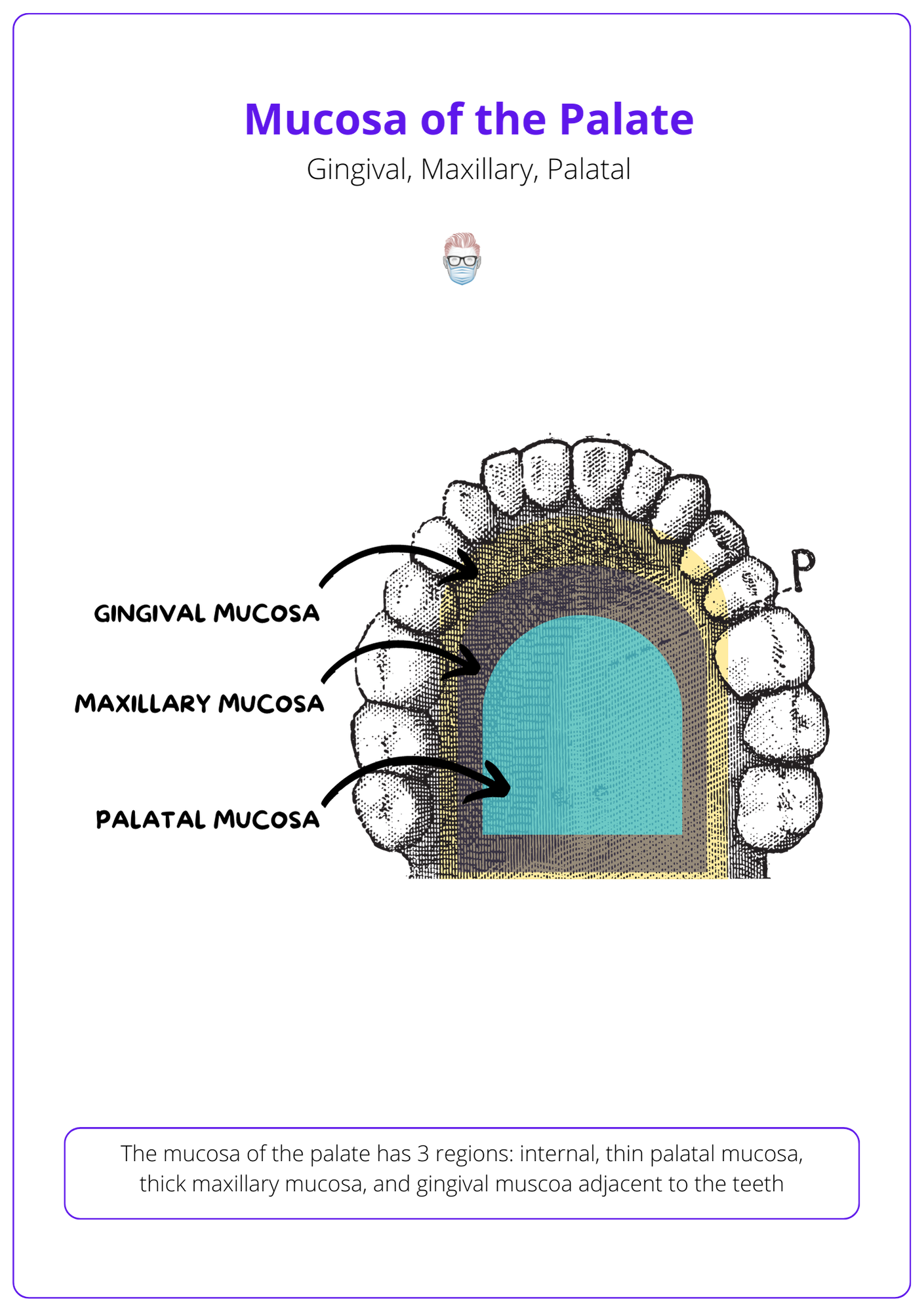
Mucosa
A mucoperiosteal layer covers the hard palate in 3 zones.
- Central Zone: thin palatal mucosa on the horizontal palate that grows the shelves before they rotate horizontally.
- Middle Zone: thick maxillary mucosa on the curved aspect of the palate that assists with maxillary growth.
- Outer Zone: gingival mucosa adjacent to the teeth.
These mucosal zones of the palate are visualised in the image below.
Foramina/Canals
There are three main portals into the hard palate:
- Incisive foramen: course of the nasopalatine nerve.
- Greater palatine foramen: located medial to 3rd molar tooth, location of greater palatine nerve and vessels.
- Lesser palatine foramen: located in the pyramidal process of the palatine bone and is the course of the lesser palatine nerve.
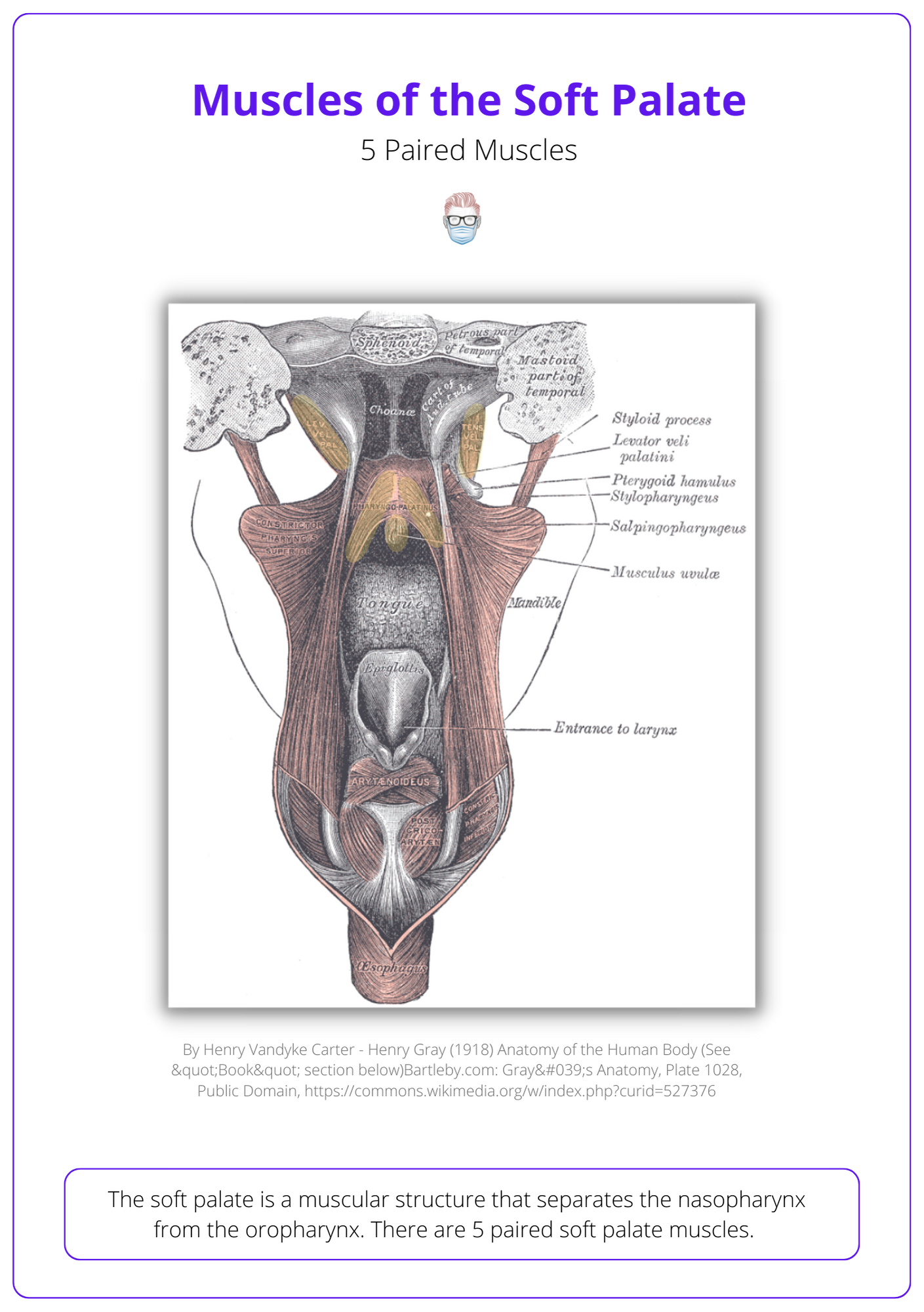
Soft Palate
The soft palate is composed of 5 paired muscles innervated by the pharyngeal plexus and trigeminal nerve. These muscles are involved in the cleft palate.
The soft palate is a muscular structure that separates the nasopharynx from the oropharynx. There are 5 paired soft palate muscles. They are all innervated by the pharyngeal plexus (IX, X and cranial part of XI), except for tensor veli palitini (trigeminal) and muscular uvulae (lesser palatine nerve).
See the below image to get a better idea of the muscles of the soft palate.
Tensor Veli Palitini (TVP)
- Origin: membranous wall of the Eustachian tube and sphenoid bone.
- Insertion: posterior hard palate.
- Function: form palatal aponeurosis, eustachian tube opening.
Levator Veli Palitini
This is the main functional muscle of the soft palate.
- Origin: temporal bone and eustachian tube.
- Insertion: posterior palatine aponeurosis.
- Function: forms muscle sling for posterior elevation of the soft palate, which closes the space between the nasopharynx and oropharynx.
Muscularis uvulae
This muscle may be absent in patients with a submucous cleft.
- Origin + Insertion: found within the uvulae (tip, it's in the name!)
- Function: elevates and shorterns the uvulae.
Palatopharyngeus
- Origin: posterior pharynx (superior thyroid cartilage, superior pharyngeal constrictor).
- Insertion: anterior velum (oral side of levator).
- Function: depresses the soft palate, elevates and constricts the oropharnyx.
Palatoglossus
- Origin: tongue (tip, it's in the name!)
- Insertion: velum (more specifically, the LVP).
- Function: depresses the soft palate and pulls anteriorly.
Other muscles involved in the pharyngeal movement include:
- Superior Pharyngeal Constrictor: movement of lateral pharyngeal wall.
- Salpingopharyngeus: does not contribute to velopharyngeal closure.
- Stylopharyngeus: does not contribute to velopharyngeal closure.
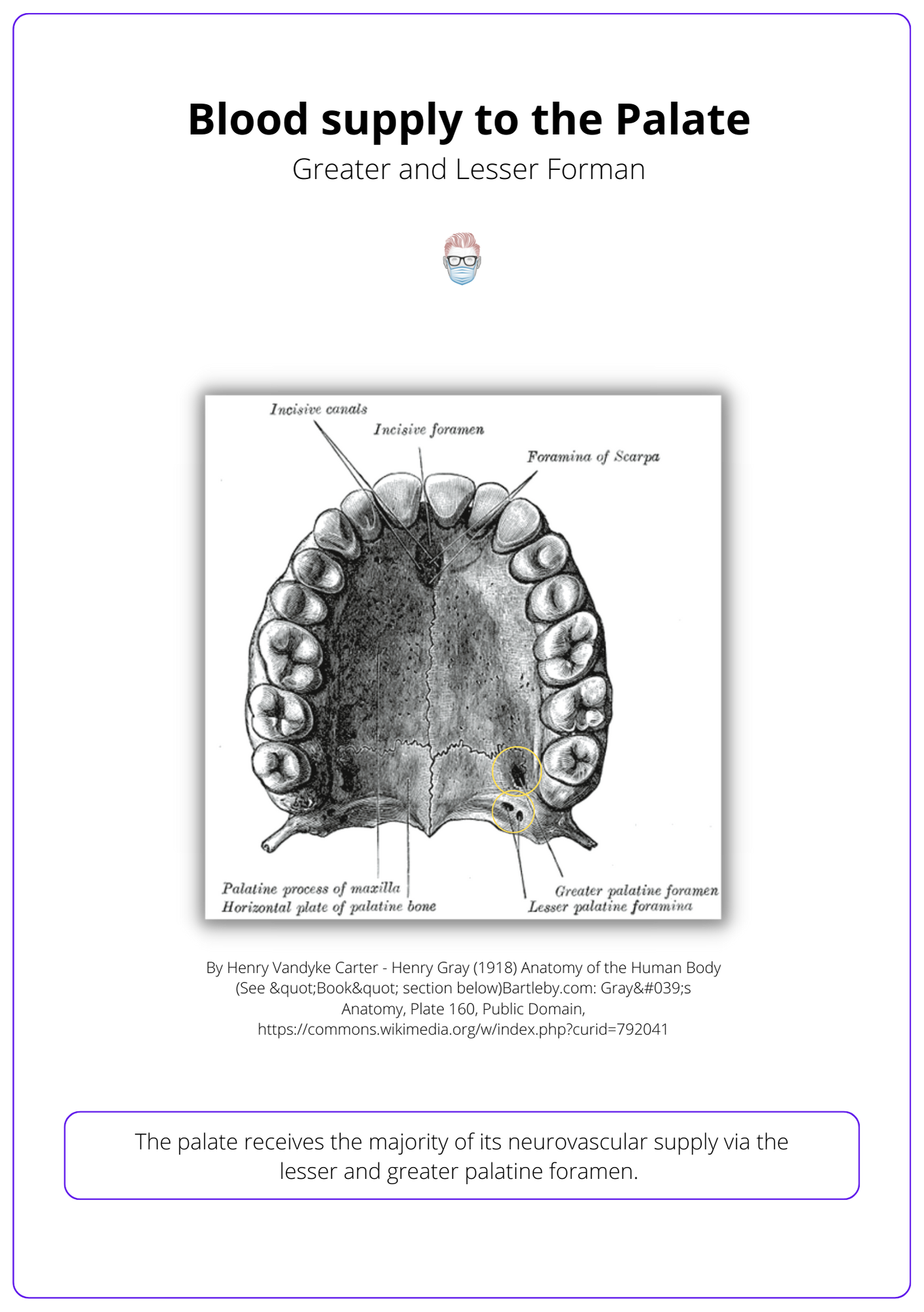
Neurovascular Supply
The palate receives is supplied primarily by the greater palatine artery and nerve, and the lesser palatine artery and nerve.
The palate receives arterial supply primarily from the greater palatine artery and the lesser palatine artery through the greater and lesser palatine foramen.
Collateral supply is received from other arteries, as detailed below. Venous drainage is into the pterygoid venous plexus.
The below image visualizes this.
Hard Palate
Greater Palatine Nerve and Artery
- Origin: Trigeminal nerve & Maxillary Artery (via descending palatine artery).
- Function: hard palate sensation and vascular supply.
- Location: travels through the greater palatine foramen.
Nasopalatine Nerve and Artery
- Origin: Trigeminal Nerve and Maxillary artery via the sphenopalatine artery.
- Location: joins greater palatine artery and nerve at the incisive foramen.
- Function: sensation and vascular supply to the premaxilla.
Anterior and Posterior Superior Alveolar Arteries
- Origin: anterior via maxillary and infraorbital, posterior via maxillary artery.
- Function: Supplies anterior and posterior alveoli.
Soft Palate
Lesser Palatine
- Origin: maxillary artery via desceding palatine artery and trigeminal nerve.
- Function: soft palate sensation and vascular supply.
- Location: travel through the lesser palatine formen.
Soft palate also receives a major blood supply from the asecending pharygngeal (from external carotid artery) and ascending palatine arteries (from facial artery).
Embryology of the Palate
Palate forms during the second month of gestation as mandible grows, tongue descends and shelves turn horizontal.
The palate begins to grow intrauterine at weeks 7-10 of gestation.
- Head and mandible grows.
- Tongue descends downwards.
- Palatal shelves rotate upwards from a vertical to a horizontal position.
- Vomer and palatal shelves fuse at incisive foramen via epithelial apoptosis.
- Primary and secondary palate fuse proximally and distally away from incisive foramen, respectively.
Males and right-sided palatal shelves become horizontal before females and left-sided palate shelves. This can explain the increased incidence of females and left-sided clefts.
The below image shows the development of palatal shelves.
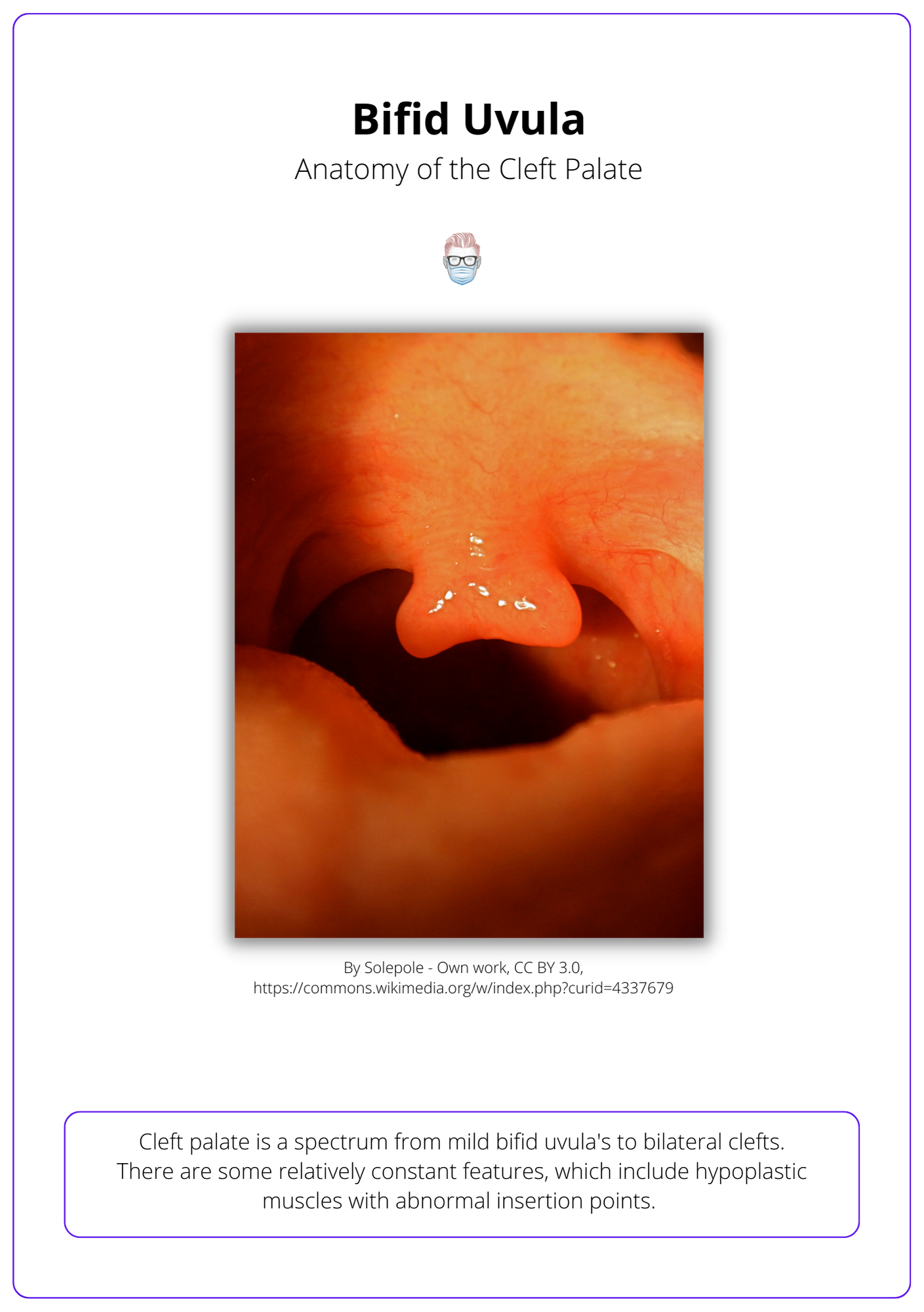
Cleft Palate Anatomy
Cleft palate is a spectrum of abnormal muscular and bony anatomy releating to the hard and soft palate.
Cleft palate is a spectrum from mild bifid uvula's to bilateral clefts. Generally speaking, there are abnormal insertions of the tensor and levator veli palitini:
- TVP: inserts into bony margins of the cleft instead of the posterior border of the hard palate.
- LVP: inserts into TVP aponeurosis.
These muscles run parallel to the cleft margin and do not join in the middle to form a sling. As a result, there is dysfunction of the velopharyngeal and eustachian tubes.
See the image below for a visualization of the Bifid Uvula.
Conclusion
1. Palate Anatomy: Gained an understanding of the hard and soft palate anatomy, including the role of the maxilla and palatine bones, the mucosal zones, and the unique muscular structure of the soft palate.
2. Neurovascular Supply: Acquired knowledge on the primary neurovascular supply to the palate, the importance of the greater and lesser palatine arteries, and nerves in the palatal region's function and health.
3. Embryological Development: Learned about the critical stages of palate formation during gestation, the process leading to the horizontal positioning of the palatal shelves, and the significance of these events in normal palate development.
4. Cleft Palate: Explored the spectrum of cleft palate anatomy, understanding how it presents a range of muscular and bony abnormalities that affect both the hard and soft palate, along with the implications for velopharyngeal and eustachian tube function.
5. Surgical Implications: Highlighted the complexity of cleft palate correction, which involves not just the repair of physical abnormalities but also the restoration of functional integrity to the affected regions.


