In this Article
Definition of Distraction Osteogenesis
Craniofacial distraction osteogenesis is the gradual and incremental traction force/tension to surgically separated bony segments to produce additional bone.
Craniofacial Distraction osteogenesis represents one of the first examples of surgically induced tissue engineering. The distraction causes a release of biological factors to generate tissue (bone and soft tissue).
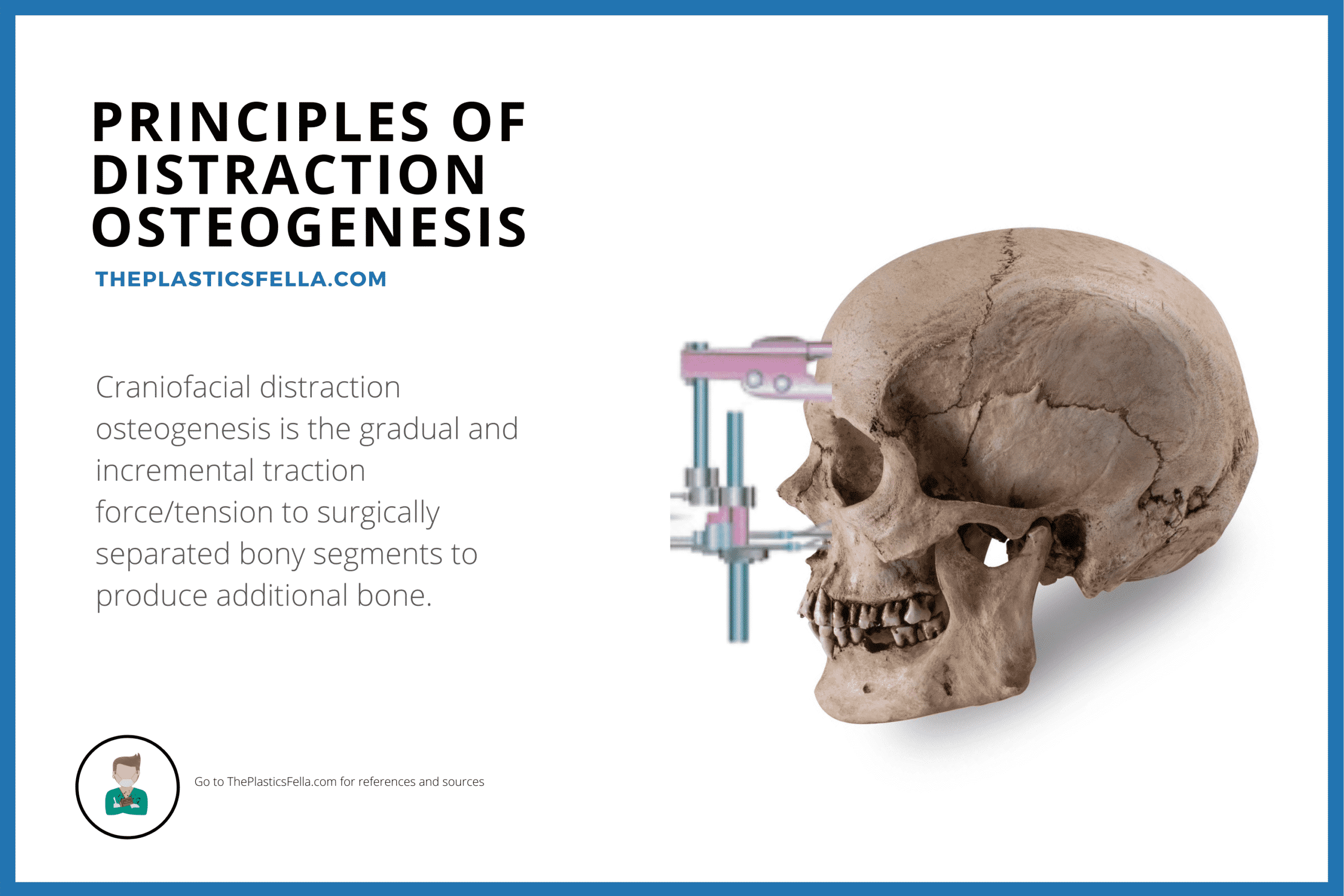
As our understanding of this technique advances, it has become a replacement for traditional techniques of bone grafting and allopatric materials in craniofacial surgery.
History of Distraction Osteogenesis
The concept of skeletal moulding has be practiced for a long time. The following were key moments in the development of distraction osteogenesis:
- Abbot, 1927: osteotomy of the femur and application of external traction to lengthen the lower extremity1
- Ilizarov: laboratory studies and popularized the concept of distraction osteogenesis2,3
- McCarthy, 1989: applied the technique to craniofacial skeleton in a series of canine mandible studies4,5
Principles of Distraction Osteogenesis
In Brief:
- 4 steps: distraction zone, latency, activation, consolidation.
- 3 types: unifocal, bifocal, trifocal
- 4 changes: fibrous, transition, remodelling, mature zone.
Steps of Distraction Osteogenesis
The principles of distraction osteogenesis can be simplified into 4 periods.
- Creation of a distraction zone: a bony separation is created by a full- thickness osteotomy or by a low-energy corticotomy (sparing the endosteum or marrow space). This segment of “free” bone is called the distraction zone and is influenced by the rigidity of the distraction device, applied distraction forces, and properties of all of the local soft tissues.
- Latency Period: Over a period of 5-7 days, the distraction zone begins to repair itself through callous formation.
- Activation Period: Tension and distraction forces are applied to elongate the intersegmentary callus. This vector of distraction should be parallel to the orientation of the device.
- Consolidation Period: External fixation maintained to allow consolidation of the newly formed bone, this is called distraction generate and can last for up to 2 months.
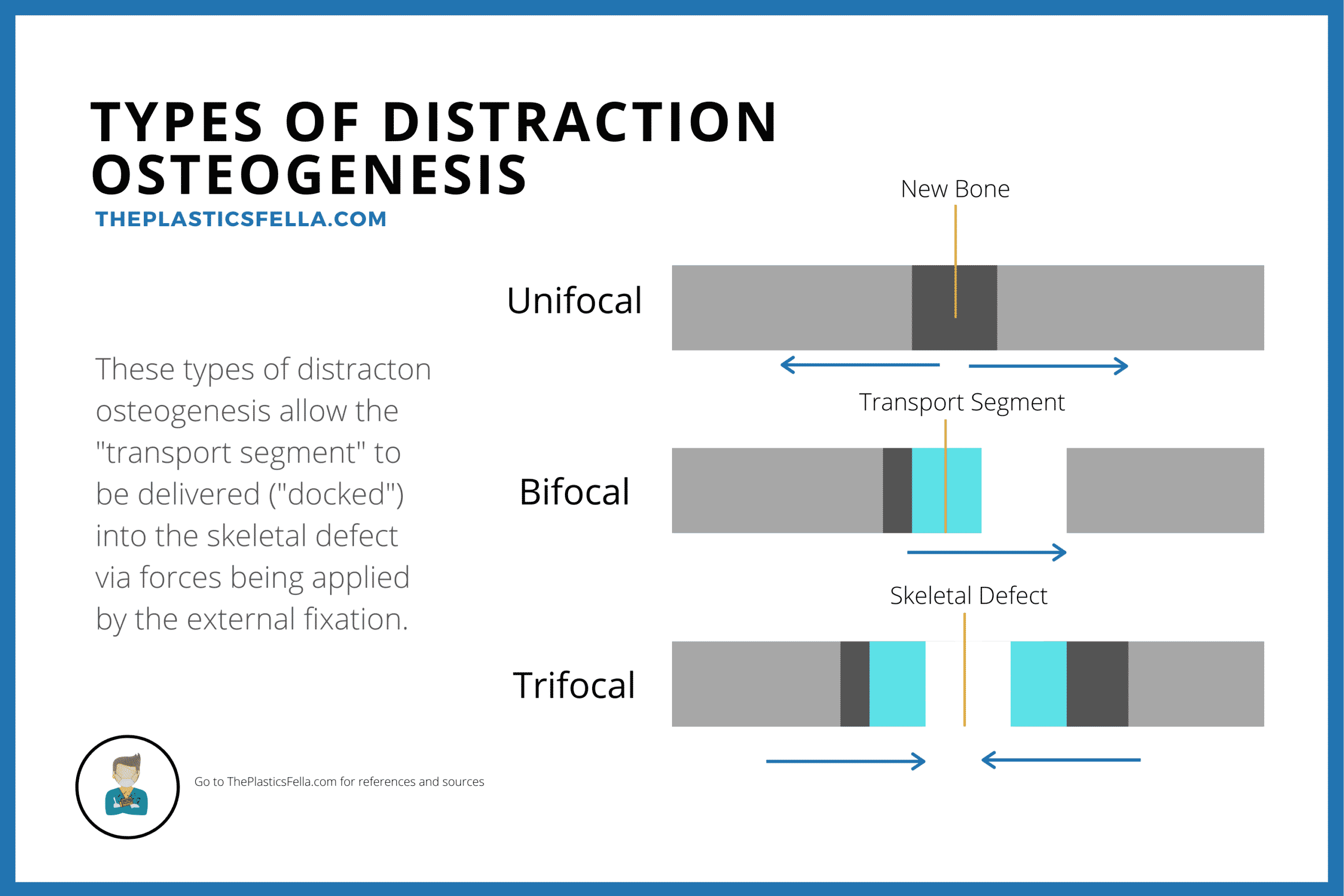
These steps allow the “transport segment” to be delivered (“docked”) into the skeletal defect from forces being applied by the external fixation. This is the key concept in craniofacial distraction osteogenesis
Types of Distraction Osteogenesis
There are 3 common types of distraction osteogenesis:
- Unifocal: single osteotomy with distraction forces applied by a device attached by screws on either side of the osteotomy;
- Bifocal: a single osteotomy with one set of pins adjacent to the osteotomy and the other set on the distal side of a skeletal defect, with a single distraction device spanning the transport segment.
- Trifocal: two osteotomies used to fill a skeletal defect in a bidirectional manner with a spanning distraction device.
These types of distraction osteogenesis used in craniofacial surgery can be visualised in the diagram below:
Histological Changes in Distraction Osteogenesis
Traditionally, the histological changes that occur during distraction osteogenesis can be classified into 4 “zones”:
- Fibrous central zone: During this time, there is mesenchymal proliferation and the fibrous bundles are longitudinally oriented
- Transition Zone: osteoids begin to form in the distraction gap along the collagen bundles.
- Remodelling Zone: Osetoclast formation and remodelling of the newly formed bone
- Mature Zone
The process by which mechanical forces are converted to cellular signals is termed mechanical transduction.
Mandibular Distraction Osteogenesis
In Brief:
- Indications: Functional & Aesthetic in patients with facial dysmorphism, respiratory issues.
- Techniques: Transcutaneous or intra-oral incisions with external or buried devices.
- Benefit to Osteotomies: earlier surgery, less complications, less relapse.
Indications
The indications of mandibular distraction in craniofacial are functional and aesthetic.
- Patients with respiratory functional problems and facial dysmorphism in such conditions as craniofacial microsomia, developmental micrognathia, Pierre Robin, and Treacher Collins syndrome
- Post-ablative mandibular defects and temporomandibular joint ankylosis
- Alveolar ridge distraction is indicated to increase alveolar ridge bone volume for the insertion of dental implants or for orthodontic tooth movements
- Infant or young patient with sleep apnea and the associated alimentary problems of eating and swallowing.
Techniques
- Mandible is approached by individual or combined trans-cutaneous (submandibular) or intraoral incisions.
- Types of devices include external (extraoral) and a buried (intraoral) device. Literature suggests more consistent results with extra-oral devices.
Comparison to Traditional Osteotomies
- Distraction allows earlier access to surgery
- Reduction in operative length, operative complications (e.g transfusions) and less secondary surgery (e.g bone grafts).
- An associated expansion or lengthening of the overlying soft tissues and muscles (distraction histiogenesis).
- In the longer term, the relapse rate is lower
Maxillary Distraction
In Brief:
- Indications: Maxillary Le Fort 1 distraction for Maxillary Retrusion
- Techniques: External (RED) frame is common
- Treatment Endpoint: Class 2 Malocclusion
Indications
Maxillary Le Fort I distraction is indicated for the correction of maxillary retrusion, as seen in:
- Cleft Lip and Palate
- Craniofacial Microsomia (can be treated with combined maxilla-mandibular distraction)
Techniques
Several types of maxillary distraction devices are available:
- External head frame (RED): relative stability and the ability to change the vector during activation
- Buried or intraoral devices are also available.
The treatment end-point:
- Class II malocclusion
- Overjet in the growing child (“overcorrection”)
Advantages of Maxillary Distraction
- Distraction allows earlier access to surgery
- Secondary maxillary advancement is often required at a later age (late teenage years).
Midface Distraction
In Brief:
- Indications: Maxillary Le Fort III distraction for midface retrusion, respiratory issues, malocclusion and severe dysphmorphism.
- Techniques: Head frames or external devices.
- Treatment: Successful in increasing airway space, distraction. Requires second operation once sketeal growth is complete.
Indications
Midface distraction is especially indicated in the syndromic craniofacial synostosis patient with:
- Exorbitism
- Malocclusion
- Sleep apnea
- Midface retrusion
- Severe dysmorphism.
Patients with orbitofacial clefts are also candidates.
Techniques
- There are two types of available distraction devices: head frames and buried devices that can be directly applied to the craniofacial skeleton through a coronal incision
- The ideal vector of distraction is in an anterior direction along a plane parallel to the maxillary occlusal surface.
- Treatment end points in the growing child include overcorrection with an overjet or class II occlusion and maximal orbito-zygomatic advancement.
Advantages of Maxillary Distraction
- Avoids the need for bone grafts and the application of plates and screws.
- Reduced operative time, requirement for transfusions and length of stay.
- Promising aesthetic results
- Greater level of distraction, bone deposition and airway space
NB: A second midface procedure will be required after the patient completes craniofacial skeletal growth. This is usually in late adolescence.
References
- Abbott L, Saunders J. THE OPERATIVE LENGTHENING OF THE TIBIA AND FIBULA: A PRELIMINARY REPORT ON THE FURTHER DEVELOPMENT OF THE PRINCIPLES AND TECHNIC. Ann Surg. 1939;110(6):961-991. doi:10.1097/00000658-193912000-00001
- Ilizarov G. The principles of the Ilizarov method. Bull Hosp Jt Dis Orthop Inst. 1988;48(1):1-11. https://www.ncbi.nlm.nih.gov/pubmed/2840141
- Ilizarov G. The possibilities offered by our method for lengthening various segments in upper and lower limbs. Basic Life Sci. 1988;48:323-324. doi:10.1007/978-1-4684-8712-1_43
- Karp N, Thorne C, McCarthy J, Sissons H. Bone lengthening in the craniofacial skeleton. Ann Plast Surg. 1990;24(3):231-237. doi:10.1097/00000637-199003000-00007
- Karp N, McCarthy J, Schreiber J, Sissons H, Thorne C. Membranous bone lengthening: a serial histological study. Ann Plast Surg. 1992;29(1):2-7. doi:10.1097/00000637-199207000-00002


